Association between PM2.5 air pollution, temperature, and sunlight during different infectious stages with the case fatality of COVID-19 in the United Kingdom: a modeling study
et al., medRxiv, doi:10.1101/2023.04.07.23288300, Apr 2023
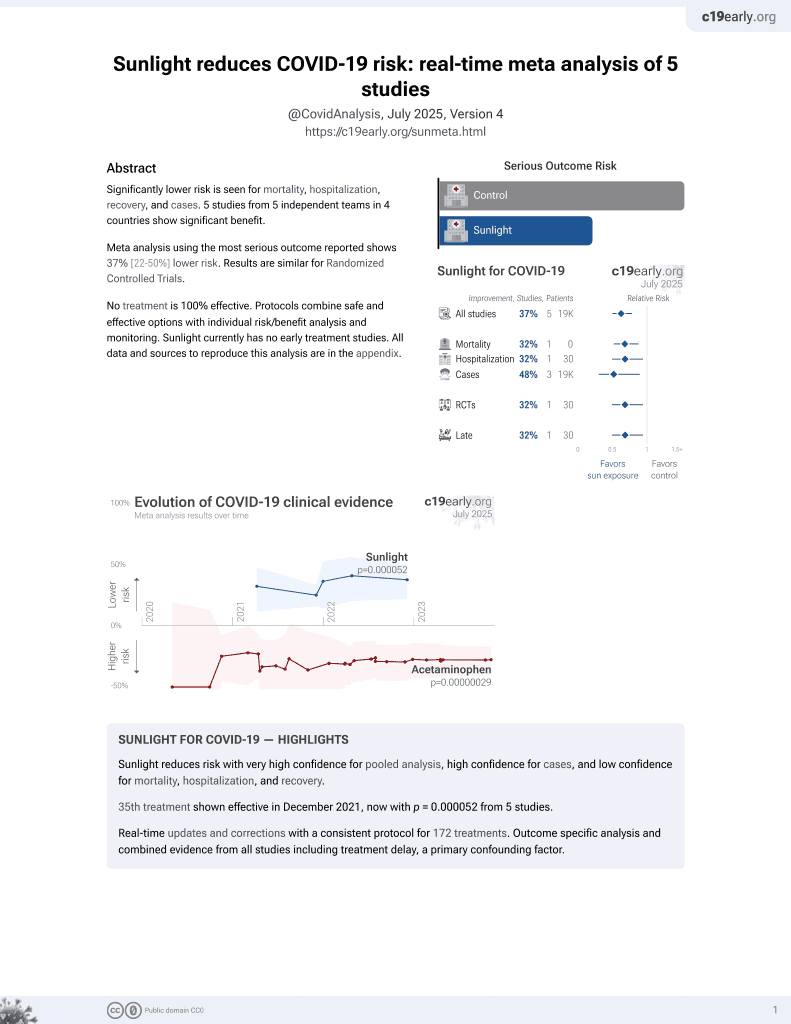
Sunlight for COVID-19
36th treatment shown to reduce risk in
December 2021, now with p = 0.000052 from 5 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
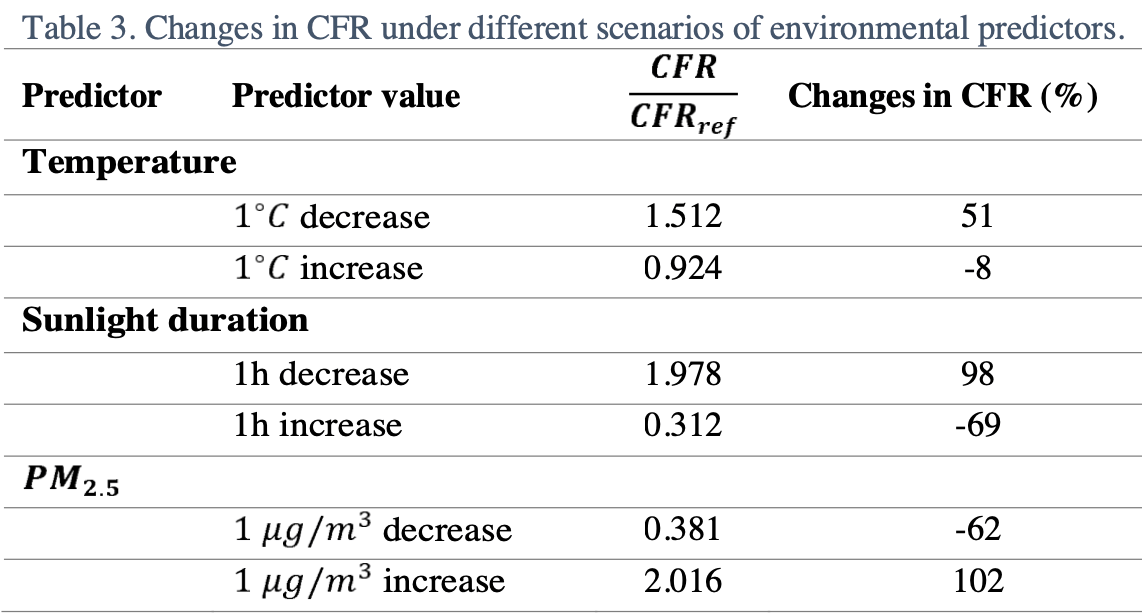
Modeling of COVID-19 cases in the UK predicting 69% lower mortality for one hour increased sunlight duration.
The model predicts lower risk with increased sunlight exposure prior to about 7 days after infection, and increased risk after 7 days. The accuracy of the 7 day estimate may be limited due to the estimation of t1, t2, and t3. We also note that the increase seen more than 7 days after infection for increased temperature and sunlight is not seen in the authors' earlier European study (with results for temperature only1).
Hossain et al., 9 Apr 2023, retrospective, United Kingdom, preprint, 4 authors, study period 26 March, 2020 - 12 May, 2020.
Contact: sean.yuan@cityu.edu.hk.
Association between PM2.5air pollution, temperature, and sunlight during different infectious stages with the case fatality of COVID-19 in the United Kingdom: a modeling study
doi:10.1101/2023.04.07.23288300
Although the relationship between the environmental factors such as weather conditions and air pollution and COVID-19 case fatality rate (CFR) has been found, the impacts of these factors to which infected cases are exposed at different infectious stages (e.g., virus exposure time, incubation period, and at or after symptom onset) are still unknown. Understanding this link can help reduce mortality rates. During the first wave of COVID-19 in the United Kingdom (UK), the CFR varied widely between and among the four countries of the UK, allowing such differential impacts to be assessed. We developed a generalized linear mixed-effect model combined with distributed lag nonlinear models to estimate the odds ratio of the weather factors (i.e., temperature, sunlight, relative humidity, and rainfall) and air pollution (i.e., ozone, ܱܰ ଶ , ܱܵ ଶ , ,ܱܥ ܯܲ ଵ and ܯܲ ଶ.ହ ) using data between March 26, 2020 and May 12, 2020 in the UK. After retrospectively time adjusted CFR was estimated using back-projection technique, the stepwise model selection method was used to choose the best model based on Akaike information criteria (AIC) and the closeness between the predicted and observed values of CFR. We found that the low temperature (8-11 ל ,)ܥ prolonged sunlight duration (11-13hours) and increased ܯܲ ଶ.ହ (11-18 ߤ݃/݉ ଷ ) after the incubation period posed a greater risk of death (measured by odds ratio (OR)) than the earlier infectious stages. The risk reached its maximum level when the low temperature occurred one day after (OR = 1.76; 95% CI: 1.10-2.81), prolonged sunlight duration 2-3 days after (OR = 1.50; 95% CI: 1.03-2.18) and increased ܯܲ ଶ.ହ at the onset of symptom (OR =1.72; 95% CI: 1.30-2.26). In contrast, prolonged sunlight duration showed a protective effect during the incubation period or earlier. After reopening, many COVID-19 cases will be identified after their symptoms appear. The findings highlight the importance of designing different preventive measures against severe illness or death considering the time before and after symptom onset.
Statement and Declarations
Competing Interest The authors have no relevant financial or non-financial interests to disclosed.
Author Contributions All authors contributed to the study conception and design. The first draft of the manuscript was written by M Pear Hossain and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
M. Pear Hossain
Ethics approval The current study did not need any ethical approval since no animal model or organ was not used in this study.
Consent to publish All authors give their consent to publish this article.
References
Becker, Watson, Carlin, A method of non parametric back projection and its application to aids data, Stat Med, doi:10.1002/sim.4780101005
Benedetti, Pachetti, Marini, Ippodrino, Gallo et al., Inverse correlation between average monthly high temperatures and COVID-19-related death rates in different geographical areas, J Transl Med, doi:10.1186/s12967
Bourdrel, Annesi-Maesano, Alahmad, Maesano, Bind, The impact of outdoor air pollution on COVID-19: a review of evidence from in vitro, animal, and human studies, European Respiratory Review, doi:10.1183/16000617.0242-2020
Chamary, Light Kills Coronavirus. Here's How It Could Help Beat Covid-19
Christophi, Sotos-Prieto, Lan, Delgado-Velandia, Efthymiou et al., Ambient temperature and subsequent COVID-19 mortality in the OECD countries and individual United States, Sci Rep, doi:10.1038/s41598-021-87803-w
Fajnzylber, Regan, Coxen, Corry, Wong et al., SARS-CoV-2 viral load is associated with increased disease severity and mortality, Nat Commun, doi:10.1038/s41467-020-19057-5
Frontera, Martin, Vlachos, Sgubin, Regional air pollution persistence links to COVID-19 infection zoning, Journal of Infection
Gasparrinia, Armstrong, Kenward, Distributed lag non-linear models, Stat Med, doi:10.1002/sim.3940
Gov, Uk, Deaths in the UK | Coronavirus in the UK
Gurka, Kelley, Edwards, Fixed and random effects models, Wiley Interdiscip Rev Comput Stat, doi:10.1002/wics.201
Haddad, Hahn, Natural and synthetic sources of circulating 25-Hydroxyvitamin D in man, Nature, doi:10.1038/244515a0
Hardie, Fletcher, Secombes, Effect of temperature on macrophage activation and the production of macrophage activating factor by rainbow trout (Oncorhynchus mykiss) leucocytes, Dev Comp Immunol, doi:10.1016/0145-305X(94)90252-6
Hart, Gorman, Jj, Modulation of the immune system by UV radiation: More than just the effects of vitamin D?, Nat Rev Immunol, doi:10.1038/nri3045
Hassan, Renfro, Blake, Rath, Durdik, Effect of temperature on functional activity of macrophages in three different species, The Journal of Immunology
Higgins-Dunn, The, has identified a new Covid-19 strain that spreads more quickly
Laird, Rhodes, Kenny, Vitamin D and Inflammation: Potential Implications for Severity of Covid-19, Ir Med J
Leaf, Ginde, Vitamin D3 to Treat COVID-19: Different Disease, Same Answer, JAMA -Journal of the American Medical Association, doi:10.1001/jama.2020.26850
Lee, Lee, The Relationship Between Indoor and Outdoor Temperature in Two Types Of Residence, Energy Procedia
Liang, Shi, Zhao, Liu, Sarnat et al., Urban Air Pollution May Enhance COVID-19 Case-Fatality and Mortality Rates in the United States, The Innovation, doi:10.1016/J.XINN.2020.100047
Liang, Yuan, Assessing the impact of temperature and humidity exposures during early infection stages on case-fatality of COVID-19: A modelling study in Europe, Environ Res, doi:10.1016/J.ENVRES.2022.112931
Ma, Zhao, Liu, He, Wang et al., Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China, Science of the Total Environment, doi:10.1016/j.scitotenv.2020.138226
Maglio, Paz, Leoni, Sunlight Effects on Immune System: Is There Something Else in addition to UV-Induced Immunosuppression?, Biomed Res Int, doi:10.1155/2016/1934518
Martelletti, Martelletti, Air Pollution and the Novel Covid-19 Disease: a Putative Disease Risk Factor, SN Compr Clin Med, doi:10.1007/S42399-020-00274-4/FIGURES/4
Martineau, Forouhi, Vitamin D for COVID-19: a case to answer?, Lancet Diabetes Endocrinol, doi:10.1016/S2213-8587(20)30268-0
Mcnoldy, Calculate Temperature, Dewpoint, and Relative Humidity Calculator
Mecenas, Bastos, Da, Vallinoto, Normando, Effects of temperature and humidity on the spread of COVID-19: A systematic review, PLoS One, doi:10.1371/journal.pone.0238339
Mendy, Wu, Keller, Fassler, Apewokin et al., Air pollution and the pandemic: Long-term PM2.5 exposure and disease severity in COVID-19 patients, Respirology, doi:10.1111/RESP.14140
Meo, Abukhalaf, Sami, Hoang, Effect of environmental pollution PM2.5, carbon monoxide, and ozone on the incidence and mortality due to SARS-CoV-2 infection in London, United Kingdom, J King Saud Univ Sci
Merzon, Tworowski, Gorohovski, Vinker, Cohen et al., Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study, FEBS J, doi:10.1111/febs.15495
Meyer, Held, Höhle, Spatio-temporal analysis of epidemic phenomena using the R package surveillance, J Stat Softw, doi:10.18637/jss.v077.i11
Panagiotou, Tee, Ihsan, Athar, Marchitelli et al., Low serum 25-hydroxyvitamin D (25[OH]D) levels in patients hospitalized with COVID-19 are associated with greater disease severity, Clin Endocrinol (Oxf)
Ratnesar ; Shumate, Williams, Green, Krause, Holland et al., Simulated Sunlight Rapidly Inactivates SARS-CoV-2 on Surfaces, J Infect Dis, doi:10.1111/cen.14276
Schultze, Aschenbrenner, COVID-19 and the human innate immune system, Cell, doi:10.1016/j.cell.2021.02.029
Stieb, Evans, To, Lakey, Shiraiwa et al., Within-City variation in reactive oxygen species from fine particle air pollution and COVID-19, Am J Respir Crit Care Med, doi:10.1164/RCCM.202011-4142OC/SUPPL_FILE/DISCLOSURES.PDF
Tank, Wijngaard, Können, Böhm, Demarée et al., Daily dataset of 20th-century surface air temperature and precipitation series for the European Climate Assessment, International Journal of Climatology, doi:10.1002/joc.773
Travaglio, Yu, Popovic, Selley, Leal et al., Links between air pollution and COVID-19 in England, Environmental Pollution, doi:10.1016/J.ENVPOL.2020.115859
Woodby, Arnold, Valacchi, SARS-CoV-2 infection, COVID-19 pathogenesis, and exposure to air pollution: What is the connection?, Ann N Y Acad Sci, doi:10.1111/NYAS.14512
Wu, Jing, Liu, Ma, Yuan et al., Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries, Science of the Total Environment, doi:10.1016/j.scitotenv.2020.139051
Wu, Nethery, Sabath, Braun, Dominici, Air pollution and COVID-19 mortality in the United States: Strengths and limitations of an ecological regression analysis, Sci Adv, doi:10.1126/SCIADV.ABD4049/SUPPL_FILE/ABD4049_SM.PDF
Yisak, Ewunetei, Kefale, Mamuye, Teshome et al., Effects of Vitamin D on COVID-19 Infection and Prognosis: A Systematic Review, Risk Manag Healthc Policy, doi:10.2147/RMHP.S291584
Zhu, Zhu, Wang, Meng, Wang et al., The association between ambient temperature and mortality of the coronavirus disease 2019 (COVID-19) in Wuhan, China: a time-series analysis, BMC Public Health, doi:10.1186/S12889-020-10131-7/TABLES/3
DOI record:
{
"DOI": "10.1101/2023.04.07.23288300",
"URL": "http://dx.doi.org/10.1101/2023.04.07.23288300",
"abstract": "<jats:p>Although the relationship between the environmental factors such as weather conditions and air pollution and COVID-19 case fatality rate (CFR) has been found, the impacts of these factors to which infected cases are exposed at different infectious stages (e.g., virus exposure time, incubation period, and at or after symptom onset) are still unknown. Understanding this link can help reduce mortality rates. During the first wave of COVID-19 in the United Kingdom (UK), the CFR varied widely between and among the four countries of the UK, allowing such differential impacts to be assessed. We developed a generalized linear mixed-effect model combined with distributed lag nonlinear models to estimate the odds ratio of the weather factors (i.e., temperature, sunlight, relative humidity, and rainfall) and air pollution (i.e., ozone, NO<jats:sub>2</jats:sub>, SO<jats:sub>2</jats:sub>, CO, PM<jats:sub>10</jats:sub>and PM<jats:sub>2.5</jats:sub>) using data between March 26, 2020 and May 12, 2020 in the UK. After retrospectively time adjusted CFR was estimated using back-projection technique, the stepwise model selection method was used to choose the best model based on Akaike information criteria (AIC) and the closeness between the predicted and observed values of CFR. We found that the low temperature (8-11<jats:sup>&#8728</jats:sup>; C), prolonged sunlight duration (11-13hours) and increased PM<jats:sub>2.5</jats:sub>(11-18μg/m<jats:sup>3</jats:sup>) after the incubation period posed a greater risk of death (measured by odds ratio (OR)) than the earlier infectious stages. The risk reached its maximum level when the low temperature occurred one day after (OR = 1.76; 95% CI: 1.10-2.81), prolonged sunlight duration 2-3 days after (OR = 1.50; 95% CI: 1.03-2.18) and increased PM<jats:sub>2.5</jats:sub>at the onset of symptom (OR =1.72; 95% CI: 1.30-2.26). In contrast, prolonged sunlight duration showed a protective effect during the incubation period or earlier. After reopening, many COVID-19 cases will be identified after their symptoms appear. The findings highlight the importance of designing different preventive measures against severe illness or death considering the time before and after symptom onset.</jats:p>",
"accepted": {
"date-parts": [
[
2023,
4,
9
]
]
},
"author": [
{
"ORCID": "http://orcid.org/0000-0001-5247-4820",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hossain",
"given": "M. Pear",
"sequence": "first"
},
{
"ORCID": "http://orcid.org/0000-0002-3297-4841",
"affiliation": [],
"authenticated-orcid": false,
"family": "Zhou",
"given": "Wen",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-8314-627X",
"affiliation": [],
"authenticated-orcid": false,
"family": "Leung",
"given": "Marco Y. T.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-0061-0012",
"affiliation": [],
"authenticated-orcid": false,
"family": "Yuan",
"given": "Hsiang-Yu",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
4,
10
]
],
"date-time": "2023-04-10T02:00:12Z",
"timestamp": 1681092012000
},
"deposited": {
"date-parts": [
[
2023,
4,
10
]
],
"date-time": "2023-04-10T02:00:13Z",
"timestamp": 1681092013000
},
"group-title": "Epidemiology",
"indexed": {
"date-parts": [
[
2023,
4,
10
]
],
"date-time": "2023-04-10T02:42:08Z",
"timestamp": 1681094528622
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
4,
9
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2023.04.07.23288300",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2023,
4,
9
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2023,
4,
9
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://medrxiv.org/lookup/doi/10.1101/2023.04.07.23288300"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": "Association between PM<sub>2.5</sub>air pollution, temperature, and sunlight during different infectious stages with the case fatality of COVID-19 in the United Kingdom: a modeling study",
"type": "posted-content"
}