Critical appraisal of multidrug therapy in the ambulatory management of patients with COVID-19 and hypoxemia Part I. Evidence supporting the strength of association
et al., The Japanese Journal of Antibiotics, doi:10.11553/antibiotics.78.1_2, Mar 2025
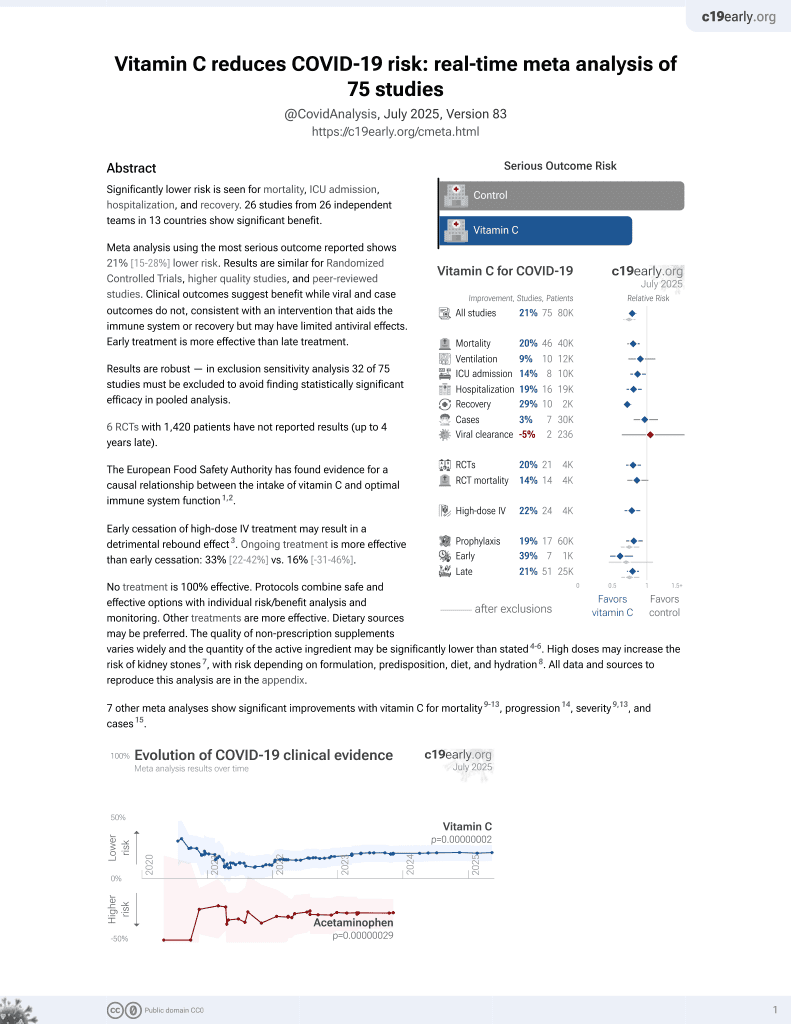
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
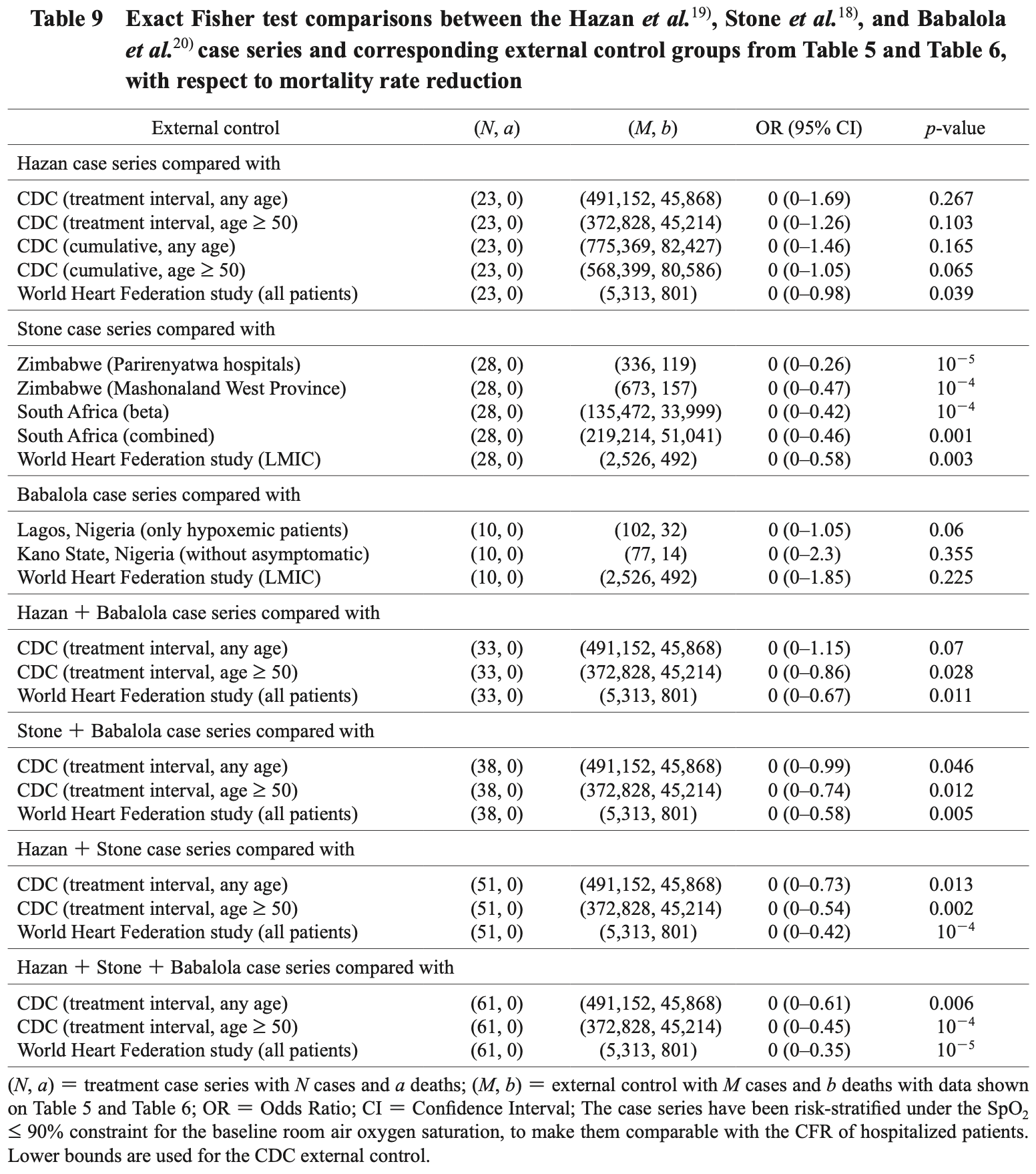
Critical appraisal of 119 COVID-19 hypoxemic patients treated with ivermectin-based multidrug protocols in the United States, Zimbabwe, and Nigeria, showing significant hospitalization rate reduction and mortality rate reduction compared to historical controls. Authors analyzed three published case series using a simplified self-controlled case series method and comparisons with external controls to investigate associations between treatment and reduced hospitalization and mortality. Of 61 patients with baseline SpO2 ≤90%, none died compared to expected mortality of 12-35% in historical controls. Protocols included combinations of ivermectin, doxycycline, zinc, vitamin C, vitamin D, and other treatments, with rapid improvement in oxygen saturation levels reported.
Gkioulekas, Ph.D. et al., 25 Mar 2025, peer-reviewed, 3 authors.
Contact: eleftherios.gkioulekas@utrgv.edu.
Critical appraisal of multidrug therapy in the ambulatory management of patients with COVID-19 and hypoxemia Part I. Evidence supporting the strength of association
doi:10.11553/antibiotics.78.1_2
This critical appraisal is focused on three published case series of 119 COVID-19 patients with hypoxemia who were successfully treated in the United States, Zimbabwe, and Nigeria with similar off-label ivermectin-based multidrug treatments that may include ivermectin, nebulized nanosilver, doxycycline, zinc, Vitamins C, and Vitamin D, resulting in rapid recovery of oxygen levels. We used a simplified self-controlled case series method to investigate the association between treatment and the existence of hospitalization rate reduction. External controls of hospitalized patients were compared against the subgroup of patients with baseline room air SpO 2 ≤ 90% to investigate the association between treatment and the existence of mortality rate reduction. No deaths were reported in any of the three case series. One case series reported 5 hospitalization equivalent events (2 ventilations and 3 uses of supplemental oxygen). Combined, the three case series comprised 119 patients of which 61 patients presented with baseline room air SpO 2 ≤ 90%. All appropriate external controls were lower-bounded by 12% case fatality rate for hospitalized patients. The existence of hospitalization rate reduction was statistically significant and resilient against both random and systemic selection bias for two out of three
Mar. 2025 and b is a lower bound of the counterfactual number of hospitalizations that would have occurred if one had followed standard hospitalization guidelines, obtained by counting the number of patients with baseline room air SpO 2 ≤ 90%. A statistically significant reduction in the hospitalization rate was inferred for the Hazan and Stone case series and for the combined Hazan + Stone, Hazan + Babalola, Stone + Babalola, and Hazan + Stone + Babalola case series. The Babalola case series, by itself, failed to achieve statistically significant hospitalization rate reduction. These comparisons are biased towards the null hypothesis of no efficacy because b underestimates the total number of counterfactual hospitalizations that would have occurred under the standard guidelines. Because of the self-controlled design, these comparisons are not susceptible to selection bias, however, hospitalization is not an entirely objective endpoint, therefore there is the possibility of some bias in the estimation of the counterfactual hospitalization rate lower bounds, which can mathematically be redefined as an equivalent selection bias in the treatment arm. The selection bias tolerance F can be used to quantify the magnitude of the gap between the random selection bias threshold and the counterfactual hospitalization rate. For the combined Hazan + Stone case series, using p 1 = 87.9% and x 1 = 21.4%, gives a selection bias tolerance F = 26.7. Including the Babalola case series, for the..
References
Adjei, Hong, Molinari, Mortality risk among patients hospitalized primarily for COVID-19 during the Omicron and Delta variant pandemic periods-United States, April 2020-June 2022, MMWR
Akinbolagbe, Otrofanowei, Akase, Predictors and outcomes of COVID-19 patients with hypoxemia in Lagos, Nigeria, J Pan Afr Thorac Soc
Babalola, Ajayi, Yunusa, Ndanusa, Ogedengbe et al., Ivermectin is associated with increase in SpO 2 in hypoxemic SARS-CoV-2 patients: pharmacodynamic profile and correlates, J Clin Chem and Lab Med
Babalola, Ndanusa, Ajayi, Ogedengbe, Thairu et al., A randomized controlled trial of ivermectin monotherapy versus hydroxychloroquine, ivermectin, and azithromycin combination therapy in COVID-19 patients in Nigeria, J Infect Dis Epidemiol
Babalola, None
Bahl, Van Baalen, Ortiz, Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort, Intern Emerg Med
Berger, Could Fisher, Jeffreys, and Neyman have agreed on testing?, Stat Sci
Borody, Clancy, Combination therapy for COVID-19 based on ivermectin in an Australian population
Boschi, Scheim, Bancod, SARS-CoV-2 spike protein induces hemagglutination: implications for COVID-19 morbidities and therapeutics and for vaccine adverse effects, Int J Mol Sci
Brouqui, Million, Parola, Mccullough, Raoult, Outcomes after early treatment with hydroxychloroquine and azithromycin: an analysis of a database of 30,423 COVID-19 patients, New Microbes New Infect
Carvallo, Hirsch, Ivermectin and herd immunity in SARS COV2 pandemic from local experience to broader possibility, Clin Immunol Res
Carvallo, Hirsch, Safety and efficacy of the combined use of ivermectin, dexamethasone, enoxaparin and aspirina against COVID-19. the I.D.E.A. protocol, J Clin Trials
Chavez, Mcgee, Mambie, COVID-19 hospital admission appropriateness analysis, Am J Biomed Sci Res
Chetty, Elucidating the pathogenesis and Rx of COVID reveals a missing element, Mod Med
Chitungo, Dzinamarira, Tungwarara, COVID-19 response in Zimbabwe: The need for a paradigm shift?, COVID
Core, R: A Language and Environment for Statistical Computing
Dayyab, Bashir, Sulaiman, Determinants of mortality among hospitalized patients with COVID-19 during first and second waves of the pandemic: a retrospective cohort study from an isolation center in Kano, Nigeria, PLoS ONE
Derwand, Scholz, Zelenko, COVID-19 outpatients-Early risk-stratified treatment with zinc plus low dose hydroxychloroquine and azithromycin: a retrospective case series study, Int J Antimicrob Agents
Gautret, Lagier, Parola, Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial, Int J Antimicrob Agents
Gkioulekas, Data and materials: critical appraisal of multi-drug therapy in the ambulatory management of patients with COVID-19 and hypoxemia, doi:10.6084/m9.figshare.24329611
Gkioulekas, Mccullough, Zelenko, Statistical analysis methods applied to early outpatient COVID-19 treatment case series data, COVID
Goodman, Toward evidence-based medical statistics. 1: The P value fallacy, Ann Intern Med
Goodman, Toward evidence-based medical statistics. 2: The Bayes factor, Ann Intern Med
Guzzo, Furtek, Porras, Safety, tolerability, and pharmacokinetics of escalating high doses of ivermectin in healthy adult subjects, J Clin Pharmacol
Hamadeh, Van Rompaey, Metreau, Eapen, New World Bank country classifications by income level
Hazan, Gunaratne, Effectiveness of ivermectin-based multidrug therapy in severely hypoxic, ambulatory COVID-19 patients, Future Microbiol
Hazan, None
Hazan, Vidal, Gkioulekas, Rapid recovery of peripheral oxygen saturation in hypoxic COVID-19 patients with ivermectin/doxycycline/zinc multidrug therapy, doi:10.6084/m9.figshare.28592639
Hill, The environment and disease: association or causation?, Proc R Soc Med
Howick, Glasziou, Aronson, The evolution of evidence hierarchies: what can Bradford Hillʼs ʻguidelines for causationʼ contribute?, JRSM
Hui, Ho, Cheung, SARS-CoV-2 Omicron variant replication in human bronchus and lung ex vivo, Nature
Jassat, Mudara, Ozougwu, Difference in mortality among individuals admitted to hospital with COVID-19 during the first and second waves in South Africa: a cohort study, Lancet Glob Health
Kass, Raftery, Bayes Factors, J Am Stat Assoc
Khan, Karim, Omicron infection enhances neutralizing immunity against the Delta variant, Nature
Knight, Ho, Pius, Risk stratification of patients admitted to hospital with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C mortality score, BMJ
Kory, Meduri, Iglesias, Varon, Cadegiani et al., MATH+ multi-modal hospital treatment protocol for COVID-19 infection: clinical and scientific rationale, J Clin Med Res
Kouamou, Matarise, Santos, Elose, Manasa, SARS-CoV-2 in Zimbabwe: milestones and challenges faced towards achieving the expected 60% herd immunity, Pan Afr Med J
Lima-Morales, Mendez-Hernandez, Flores, Effectiveness of a multidrug therapy consisting of Ivermectin, Azithromycin, Montelukast, and Acetylsalicylic acid to prevent hospitalization and death among ambulatory COVID-19 cases in Tlaxcala, Mexico, Int J Infect Dis
Lounnas, Gkioulekas, Rendell, Lacout, Azalbert et al., An independent analysis of a retrospective cohort of 30,423 Covid-19 patients treated at IHU-Mediterranean in Marseille, France: Part 1, Efficacy of early treatment with hydroxychloroquine and azithromycin, Arch Microbiol Immunol
Madamombe, Shambira, Masoja, Factors associated with COVID-19 fatality among patients admitted in Mashonaland West Province, Zimbabwe 2020-2022: a secondary data analysis, Pan Afr Med J
Marik, Kory, Varon, Iglesias, Meduri, MATH+ protocol for the treatment of SARS-CoV-2 infection: the scientific rationale, Expert Rev Anti Infect Ther
Mccullough, Alexander, Armstrong, Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19), Rev Cardiovasc Med
Mccullough, Innovative early sequenced multidrug therapy for SARS-CoV-2 (COVID-19) infection to reduce hospitalization and death, Int J Med Sci Clin Invent
Mccullough, Kelly, Ruocco, Pathophysiological basis and rationale for early outpatient treatment of SARS-CoV-2 (COVID-19) infection, Am J Med
Mcnamara, Wiegand, Burke, Estimating the early impact of the US COVID-19 vaccination programme on COVID-19 cases, emergency department visits, hospital admissions, and deaths among adults aged 65 years and older: an ecological analysis of national surveillance data, Lancet
Mejia, Medina, Cornejo, Oxygen saturation as a predictor of mortality in hospitalized adult patients with COVID-19 in a public hospital in Lima, Peru, PLoS ONE
Miklowski, Jansen, Auron, Whinney, The hospitalized patient with COVID-19 on the medical ward: Cleveland Clinic approach to management, Cleve Clin J Med
Miller, Tada, Goto, Prediction models for severe manifestations and mortality due to COVID-19: a systematic review, Acad Emerg Med
Million, Lagier, Tissot-Dupont, Early treatment with hydroxychloroquine and azithromycin in 10,429 COVID-19 outpatients: a monocentric retrospective cohort study, Rev Cardiovasc Med
Morey, Romeijn, Rouder, The philosophy of Bayes factors and the quantification of statistical evidence, J Math Psychol
Murchu, Byrne, Carty, Quantifying the risk of SARS-CoV-2 reinfection over time, Rev Med Virol
Murewanhema, Musuka, Denhere, Chingombe, Mapingure et al., The landscape of COVID-19 vaccination in Zimbabwe: a narrative review and analysis of the strengths, weaknesses, opportunities and threats of the programme, Vaccines
Nardo, Gentilotti, Mazzaferri, Multi-Criteria Decision Analysis to prioritize hospital admission of patients affected by COVID-19 in low-resource settings with hospital-bed shortage, Int J Infect Dis
Petersen, Douglas, Whitaker, Self controlled case series methods: an alternative to standard epidemiological study designs, BMJ
Poskurica, Stevanovic, Zdravkovic, Admission predictors of mortality in hospitalized COVID-19 patientsa Serbian cohort study, J Clin Med
Prabhakaran, Singh, Kondal, Cardiovascular risk factors and clinical outcomes among patients hospitalized with COVID-19: findings from the World Heart Federation COVID-19 study, Glob Heart
Rendell, Commentary on ʻStatistical analysis methods applied to early outpatient COVID-19 treatment case series dataʼ by Gkioulekas, McCullough and Zelenko: a return back to the future, J Health Care Commun
Risch, Early outpatient treatment of symptomatic, high-risk COVID-19 patients that should be ramped-up immediately as key to the pandemic crisis, Am J Epidemiol
Scheim, Parry, Rabbolini, Back to the basics of SARS-CoV-2 biochemistry: microvascular occlusive glycan bindings govern its morbidities and inform therapeutic responses, Viruses
Sterne, Some remarks on confidence or fiducial limits, Biometrika
Stone, Aldous, An ethical clinical, and regulatory analysis: Ivermectin and COVID-19 treatment in Zimbabwe
Stone, Gill, Zimbabwe rollout of Silver and Ivermectin Protocol
Stone, Gkioulekas, The Stone/Gill SID treatment protocol for COVID-19
Stone, Ndarukwa, Scheim, Changes in SpO 2 on room air for 34 severe COVID-19 patients after ivermectin-based combination treatment: 62% normalization within 24 hours, Biologics
Stone, Ndarukwa, Scheim, Rapid increase of SpO 2 on room air for 34 severe COVID-78-1 Mar. 2025 19 patients after ivermectin-based combination treatment: 55-62% normalization within 12-24 hours, doi:10.21203/rs.3.rs-1048271/v1
Stone, None
Thairu, Babalola, Ajayi, Ndanusa, Ogedengbe et al., A comparison of ivermectin and non ivermectin based regimen for COVID-19 in Abuja: effects on virus clearance, days-todischarge and mortality, J Pharm Res Int
Ward, The role of causal criteria in causal inferences: Bradford Hillʼs ʻaspects of associationʼ, Epidemiol Perspect Innov
DOI record:
{
"DOI": "10.11553/antibiotics.78.1_2",
"ISSN": [
"03682781",
"03682781",
"21865477"
],
"URL": "https://doi.org/10.11553/antibiotics.78.1_2",
"author": [
{
"family": "Gkioulekas, Ph.D.",
"given": "Eleftherios"
},
{
"family": "McCullough, M.D., M.P.H.",
"given": "Peter A."
},
{
"family": "Aldous, Ph.D.",
"given": "Colleen"
}
],
"container-title": "The Japanese Journal of Antibiotics",
"issued": {
"date-parts": [
[
2025,
3,
25
]
]
},
"language": "en",
"number": "1",
"page": "2-34",
"publisher": "Japan Antibiotics Research Association",
"title": "Critical appraisal of multidrug therapy in the ambulatory management of patients with COVID-19 and hypoxemia Part I. Evidence supporting the strength of association",
"volume": "78"
}
gkioulekas6