NLRP3 inflammasome activation and oxidative stress status in the mild and moderate SARS-CoV-2 infected patients: impact of melatonin as a medicinal supplement
et al., Zeitschrift für Naturforschung C, doi:10.1515/znc-2021-0101, Aug 2021
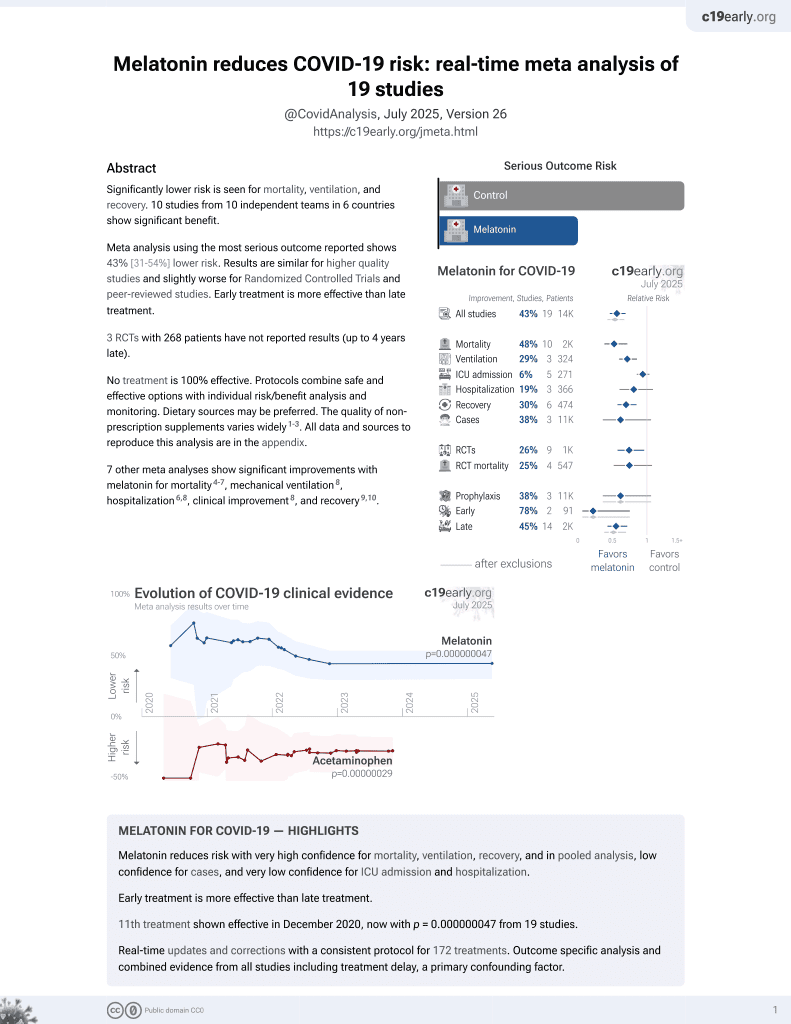
Melatonin for COVID-19
12th treatment shown to reduce risk in
December 2020, now with p = 0.0000000099 from 19 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Study of melatonin treatment in COVID-19 hospitalized patients showing anti-oxidative and anti-inflammatory activity, and beneficial impacts on lung cytokine storm.
Ghaleh et al., 5 Aug 2021, peer-reviewed, 9 authors.
NLRP3 inflammasome activation and oxidative stress status in the mild and moderate SARS-CoV-2 infected patients: impact of melatonin as a medicinal supplement
Zeitschrift für Naturforschung C, doi:10.1515/znc-2021-0101
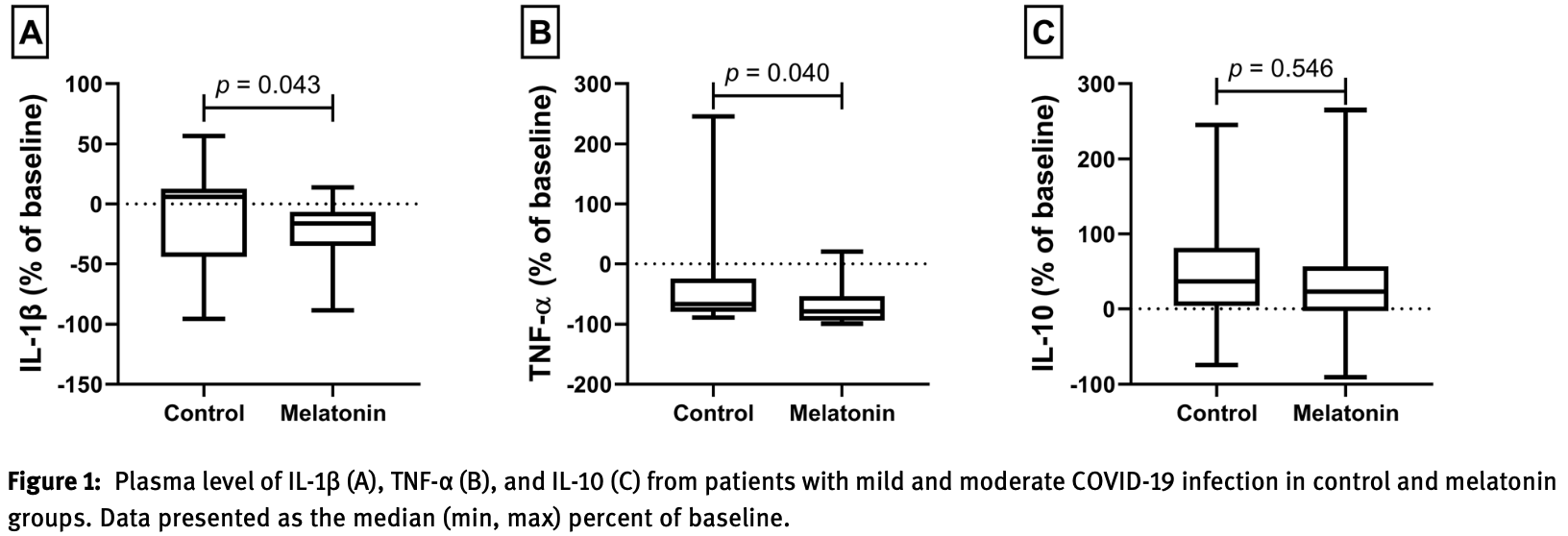
The inflammasome as a multiprotein complex has a role in activating ASC and caspase-1 resulting in activating IL-1β in various infections and diseases like corona virus infection in various tissues. It was shown that these tissues are affected by COVID-19 patients. According to the current evidence, melatonin is not veridical while possessing a high safety profile, however, it possesses indirect anti-viral actions owing to its anti-oxidation, antiinflammation, and immune improving properties. This study aims to assess the impacts of melatonin as the complementary treatments on oxidative stress agents and inflammasome activation in patients with COVID-19. Melatonin supplement (9 mg daily, orally) was provided for the patients hospitalized with a COVID-19 analysis for 14 days. For measuring IL-10, IL-1β, and TNF-α cytokines and malondialdehyde (MDA), nitric oxide (NO), and superoxide dismutase (SOD) level and the expression of CASP1 and ASC genes, blood samples were gathered from the individuals at the start and termination of the therapy. Our findings indicated that melatonin is used as a complementary treatment to reduce the levels of TNF-α and IL-1β cytokines, MDA, and NO levels in COVID-19 patients and significantly increase SOD level, however, the levels of IL-10 cytokine possesses no considerable changes. The findings revealed that genes of CASP1 and ASC were dysregulated by melatonin regulating the inflammasome complex. Based on the findings of the current study, it is found that melatonin can be effective as a medicinal supplement in decreasing the inflammasome multiprotein complex and oxidative stress along with beneficial impacts on lung cytokine storm of COVID-19 patients.
References
Akbariqomi, Hosseini, Rashidiani, Sedighian, Biganeh et al., Clinical characteristics and outcome of hospitalized COVID-19 patients with diabetes: a single-center, retrospective study in Iran, Diabetes Res Clin Pract
Alon, Sportiello, Kozlovski, Kumar, Reilly et al., Leukocyte trafficking to the lungs and beyond: lessons from influenza for COVID-19, Nat Rev Immunol
Amaral, Vinhaes, Oliveira-De-Souza, Nogueira, Akrami et al., The interplay between systemic inflammation, oxidative stress, and tissue remodeling in tuberculosis, Antioxidants Redox Signal
Arjunan, Eye on the enigmatic link: dysbiotic oral pathogens in ocular diseases; the flip side, Int Rev Immunol, doi:10.1080/08830185.2020.1845330
Beltrán-García, Osca-Verdegal, Pallardó, Ferreres, Rodríguez et al., Oxidative stress and inflammation in COVID-19-associated sepsis: the potential role of anti-oxidant therapy in avoiding disease progression, Antioxidants, doi:10.3390/antiox9100936
Choudhry, Zhao, Xu, Zanin, Yang, Chinese therapeutic strategy for fighting COVID-19 and potential smallmolecule inhibitors against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), J Med Chem
De Bruin, Lequarre, Mccourt, Clevestig, Pigazzani et al., Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic, Saf Sci
Elkodous, El-Sayyad, Mm, Engineered nanomaterials as fighters against SARS-CoV-2: the way to control and treat pandemics, Environ Sci Pollut Res Int, doi:10.1007/s11356-020-11032-3
Fang, Zhao, Xiang, Zhao, Zhong, Melatonin inhibits formation of mitochondrial permeability transition pores and improves oxidative phosphorylation of frozen-thawed ram sperm, Front Endocrinol
Favero, Franceschetti, Bonomini, Rodella, Rezzani, Melatonin as an anti-inflammatory agent modulating inflammasome activation, Internet J Endocrinol
Hasana, Hossain, Jalouli, Kabir, Uddin et al., Genetic diversity of SARS-CoV2 and environmental settings: possible association with neurological disorders, Mol Neurobiol
Huang, Cao, Liu, Shi, Wei, Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice, J Pineal Res
Huang, Cao, Wei, Melatonin decreases TLR3-mediated inflammatory factor expression via inhibition of NF-kappa B activation in respiratory syncytial virus-infected RAW264.7 macrophages, J Pineal Res
Juybari, Pourhanifeh, Hosseinzadeh, Hemati, Mehrzadi, Melatonin potentials against viral infections including COVID-19: current evidence and new findings, Virus Res
Kabir, Uddin, Hossain, Abdulhakim, Alam et al., COVID-19 pandemic: from molecular pathogenesis to potential investigational therapeutics, Front Cell Dev Biol
Land, DAMP-promoted efferent innate immune responses in human diseases: inflammation
Lee, Channappanavar, Kanneganti, Coronaviruses: innate immunity, inflammasome activation, inflammatory cell death, and cytokines, Trends Immunol
Lin, Cao, Nuclear innate sensors for nucleic acids in immunity and inflammation, Immunol Rev
Liu, Gan, Xu, Luo, Ren et al., Melatonin alleviates inflammasome-induced pyroptosis through inhibiting NF-κB/ GSDMD signal in mice adipose tissue, J Pineal Res, doi:10.1111/jpi.12414
Naggar, Giesy, Daim, Ansari, Sn et al., Fighting against the second wave of COVID-19: can honeybee products help protect against the pandemic? Saudi, J Biol Sci
Ouyang, Zhong, Lu, Zhong, Hu et al., Inhibitory effect of melatonin on Mst1 ameliorates myocarditis through attenuating ER stress and mitochondrial dysfunction, J Mol Histol
Owens, Update in pediatric sleep medicine, Curr Opin Pulm Med
Patel, Rahmani, Gandhi, Seyam, Joshi et al., Revisiting the pineal gland: a review of calcification, masses, precocious puberty, and melatonin functions, Int J Neurosci
Perez-Garmendia, De Eguileta Rodriguez, Ramos-Martinez, Zuñiga, Gonzalez-Salinas et al., Interplay between oxidative stress, inflammation, and amyloidosis in the anterior segment of the eye; its pathological implications, Oxid Med Cell Longev
Pietschmann, Mertz, Medical humanism and complementary, alternative and integrative medicine, Arch Philos
Sun, Gusdon, Qu, Effects of melatonin on cardiovascular diseases: progress in the past year, Curr Opin Lipidol
Tordjman, Chokron, Delorme, Charrier, Bellissant et al., Melatonin: pharmacology, functions and therapeutic benefits, Curr Neuropharmacol
Ueda, Park, Ochiai, Itakura, Disseminated intravascular coagulation (DIC) in rabbit haemorrhagic disease, Jpn J Vet Res
Verdonschot, Hazebroek, Merken, Debing, Dennert et al., Relevance of cardiac parvovirus B19 in myocarditis and dilated cardiomyopathy: review of the literature, Eur J Heart Fail
Vural, Van Munster, De Rooij, Optimal dosages for melatonin supplementation therapy in older adults: a systematic review of current literature, Drugs Aging
Yu, Kubota, Okita, Maeda, The anti-inflammatory and antioxidant effects of melatonin on LPS-stimulated bovine mammary epithelial cells, PLoS One
Zhang, Li, Grailer, Wang, Wang et al., Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome, J Pineal Res
DOI record:
{
"DOI": "10.1515/znc-2021-0101",
"ISSN": [
"0939-5075",
"1865-7125"
],
"URL": "http://dx.doi.org/10.1515/znc-2021-0101",
"abstract": "<jats:title>Abstract</jats:title>\n <jats:p>The inflammasome as a multiprotein complex has a role in activating ASC and caspase-1 resulting in activating IL-1β in various infections and diseases like corona virus infection in various tissues. It was shown that these tissues are affected by COVID-19 patients. According to the current evidence, melatonin is not veridical while possessing a high safety profile, however, it possesses indirect anti-viral actions owing to its anti-oxidation, anti-inflammation, and immune improving properties. This study aims to assess the impacts of melatonin as the complementary treatments on oxidative stress agents and inflammasome activation in patients with COVID-19. Melatonin supplement (9 mg daily, orally) was provided for the patients hospitalized with a COVID-19 analysis for 14 days. For measuring IL-10, IL-1β, and TNF-α cytokines and malondialdehyde (MDA), nitric oxide (NO), and superoxide dismutase (SOD) level and the expression of <jats:italic>CASP1</jats:italic> and <jats:italic>ASC</jats:italic> genes, blood samples were gathered from the individuals at the start and termination of the therapy. Our findings indicated that melatonin is used as a complementary treatment to reduce the levels of TNF-α and IL-1β cytokines, MDA, and NO levels in COVID-19 patients and significantly increase SOD level, however, the levels of IL-10 cytokine possesses no considerable changes. The findings revealed that genes of <jats:italic>CASP1</jats:italic> and <jats:italic>ASC</jats:italic> were dysregulated by melatonin regulating the inflammasome complex. Based on the findings of the current study, it is found that melatonin can be effective as a medicinal supplement in decreasing the inflammasome multiprotein complex and oxidative stress along with beneficial impacts on lung cytokine storm of COVID-19 patients.</jats:p>",
"alternative-id": [
"10.1515/znc-2021-0101"
],
"author": [
{
"affiliation": [
{
"name": "Applied Virology Research Center, Baqiyatallah University of Medical Sciences , Tehran , Iran"
}
],
"family": "Esmaeili Gouvarchin Ghaleh",
"given": "Hadi",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Department of Animal Sciences and Biotechnology, Faculty of Life Sciences and Biotechnology , Shahid Beheshti University , Tehran , Iran"
}
],
"family": "Hosseini",
"given": "Abdolkarim",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Chemical Injuries Research Center, Systems Biology and Poisonings Institute, Baqiyatallah University of Medical Sciences , Tehran , Iran"
}
],
"family": "Aghamollaei",
"given": "Hossein",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Molecular Biology Research Center, Systems Biology and Poisonings Institute, Baqiyatallah University of Medical Sciences , Tehran , Iran"
}
],
"family": "Fasihi-Ramandi",
"given": "Mahdi",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Chemical Injuries Research Center, Systems Biology and Poisonings Institute, Baqiyatallah University of Medical Sciences , Tehran , Iran"
}
],
"family": "Alishiri",
"given": "Gholamhossein",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Immunology, Faculty of Medicine , Ahvaz Jundishapur University of Medical Sciences , Ahvaz , Iran"
},
{
"name": "Abadan University of Medical Sciences , Abadan , Iran"
}
],
"family": "Saeedi-Boroujeni",
"given": "Ali",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Sabzevar University of Medical Sciences, School of Medicine , Sabzevar , Iran"
}
],
"family": "Hassanpour",
"given": "Kazem",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Thalassemia and Hemoglobinopathy Research Center, Health Research Institute, Ahvaz Jundishapur University of Medical Sciences , Ahvaz , Iran"
}
],
"family": "Mahmoudian-Sani",
"given": "Mohammad-Reza",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Applied Biotechnology Research Center, Baqiyatallah University of Medical Sciences , Tehran , Iran"
}
],
"family": "Farnoosh",
"given": "Gholamreza",
"sequence": "additional"
}
],
"container-title": "Zeitschrift für Naturforschung C",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
8,
6
]
],
"date-time": "2021-08-06T03:35:18Z",
"timestamp": 1628220918000
},
"deposited": {
"date-parts": [
[
2023,
4,
2
]
],
"date-time": "2023-04-02T09:06:25Z",
"timestamp": 1680426385000
},
"indexed": {
"date-parts": [
[
2024,
5,
9
]
],
"date-time": "2024-05-09T09:45:51Z",
"timestamp": 1715247951841
},
"is-referenced-by-count": 11,
"issue": "1-2",
"issued": {
"date-parts": [
[
2021,
8,
6
]
]
},
"journal-issue": {
"issue": "1-2",
"published-online": {
"date-parts": [
[
2021,
8,
24
]
]
},
"published-print": {
"date-parts": [
[
2022,
1,
27
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://www.degruyter.com/document/doi/10.1515/znc-2021-0101/xml",
"content-type": "application/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.degruyter.com/document/doi/10.1515/znc-2021-0101/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "374",
"original-title": [],
"page": "37-42",
"prefix": "10.1515",
"published": {
"date-parts": [
[
2021,
8,
6
]
]
},
"published-online": {
"date-parts": [
[
2021,
8,
6
]
]
},
"published-print": {
"date-parts": [
[
2022,
1,
27
]
]
},
"publisher": "Walter de Gruyter GmbH",
"reference": [
{
"DOI": "10.1080/00207454.2019.1692838",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_001",
"unstructured": "Patel, S, Rahmani, B, Gandhi, J, Seyam, O, Joshi, G, Reid, I, et al.. Revisiting the pineal gland: a review of calcification, masses, precocious puberty, and melatonin functions. Int J Neurosci 2020;130:464–75. https://doi.org/10.1080/00207454.2019.1692838."
},
{
"DOI": "10.2174/1570159X14666161228122115",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_002",
"unstructured": "Tordjman, S, Chokron, S, Delorme, R, Charrier, A, Bellissant, E, Jaafari, N, et al.. Melatonin: pharmacology, functions and therapeutic benefits. Curr Neuropharmacol 2017;15:434–43. https://doi.org/10.2174/1570159x14666161228122115."
},
{
"DOI": "10.1016/j.virusres.2020.198108",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_003",
"unstructured": "Bahrampour Juybari, K, Pourhanifeh, MH, Hosseinzadeh, A, Hemati, K, Mehrzadi, S. Melatonin potentials against viral infections including COVID-19: current evidence and new findings. Virus Res 2020;287:198108. https://doi.org/10.1016/j.virusres.2020.198108."
},
{
"DOI": "10.3389/fendo.2019.00896",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_004",
"unstructured": "Fang, Y, Zhao, C, Xiang, H, Zhao, X, Zhong, R. Melatonin inhibits formation of mitochondrial permeability transition pores and improves oxidative phosphorylation of frozen-thawed ram sperm. Front Endocrinol 2019;10:896. https://doi.org/10.3389/fendo.2019.00896."
},
{
"DOI": "10.1097/MOL.0000000000000314",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_005",
"unstructured": "Sun, H, Gusdon, AM, Qu, S. Effects of melatonin on cardiovascular diseases: progress in the past year. Curr Opin Lipidol 2016;27:408–13. https://doi.org/10.1097/mol.0000000000000314."
},
{
"DOI": "10.1097/MCP.0b013e32834ba901",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_006",
"unstructured": "Owens, JA. Update in pediatric sleep medicine. Curr Opin Pulm Med 2011;17:425–30. https://doi.org/10.1097/mcp.0b013e32834ba901."
},
{
"DOI": "10.1016/j.ssci.2020.104773",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_007",
"unstructured": "Bruinen de Bruin, Y, Lequarre, AS, McCourt, J, Clevestig, P, Pigazzani, F, Zare Jeddi, M, et al.. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf Sci 2020;128:104773. https://doi.org/10.1016/j.ssci.2020.104773."
},
{
"DOI": "10.3917/aphi.834.0083",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_008",
"unstructured": "Pietschmann, IS, Mertz, M. Medical humanism and complementary, alternative and integrative medicine. Arch Philos 2020;83:83–102. https://doi.org/10.3917/aphi.834.0083."
},
{
"DOI": "10.1021/acs.jmedchem.0c00626",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_009",
"unstructured": "Choudhry, N, Zhao, X, Xu, D, Zanin, M, Chen, W, Yang, Z, et al.. Chinese therapeutic strategy for fighting COVID-19 and potential small-molecule inhibitors against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). J Med Chem 2020;63:13205–27. https://doi.org/10.1021/acs.jmedchem.0c00626."
},
{
"DOI": "10.1016/j.diabres.2020.108467",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_010",
"unstructured": "Akbariqomi, M, Hosseini, MS, Rashidiani, J, Sedighian, H, Biganeh, H, Heidari, R, et al.. Clinical characteristics and outcome of hospitalized COVID-19 patients with diabetes: a single-center, retrospective study in Iran. Diabetes Res Clin Pract 2020;169:108467. https://doi.org/10.1016/j.diabres.2020.108467."
},
{
"DOI": "10.1016/j.sjbs.2020.12.031",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_011",
"unstructured": "Al Naggar, Y, Giesy, JP, Abdel-Daim, MM, Javed Ansari, M, Al-Kahtani, SN, Yahya, G. Fighting against the second wave of COVID-19: can honeybee products help protect against the pandemic? Saudi J Biol Sci 2021;28:1519–27. https://doi.org/10.1016/j.sjbs.2020.12.031."
},
{
"DOI": "10.1007/s11356-020-11032-3",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_012",
"unstructured": "Abd Elkodous, M, El-Sayyad, GS, Abdel-Daim, MM. Engineered nanomaterials as fighters against SARS-CoV-2: the way to control and treat pandemics. Environ Sci Pollut Res Int 2020:1–7. https://doi.org/10.1007/s11356-020-11032-3."
},
{
"DOI": "10.3389/fcell.2020.00616",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_013",
"unstructured": "Kabir, MT, Uddin, MS, Hossain, MF, Abdulhakim, JA, Alam, MA, Ashraf, GM, et al.. COVID-19 pandemic: from molecular pathogenesis to potential investigational therapeutics. Front Cell Dev Biol 2020;8:616. https://doi.org/10.3389/fcell.2020.00616."
},
{
"DOI": "10.1007/s12035-020-02239-z",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_014",
"unstructured": "Hasana, S, Hossain, MF, Jalouli, M, Kabir, MT, Uddin, MG, Wahed, MII, et al.. Genetic diversity of SARS-CoV2 and environmental settings: possible association with neurological disorders. Mol Neurobiol 2021;58:1917–31. https://doi.org/10.1007/s12035-020-02239-z."
},
{
"DOI": "10.1111/imr.12893",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_015",
"unstructured": "Lin, H, Cao, X. Nuclear innate sensors for nucleic acids in immunity and inflammation. Immunol Rev 2020;297:162–73. https://doi.org/10.1111/imr.12893."
},
{
"DOI": "10.1016/j.it.2020.10.005",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_016",
"unstructured": "Lee, S, Channappanavar, R, Kanneganti, TD. Coronaviruses: innate immunity, inflammasome activation, inflammatory cell death, and cytokines. Trends Immunol 2020;41:1083–99. https://doi.org/10.1016/j.it.2020.10.005."
},
{
"DOI": "10.1038/s41577-020-00470-2",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_017",
"unstructured": "Alon, R, Sportiello, M, Kozlovski, S, Kumar, A, Reilly, EC, Zarbock, A, et al.. Leukocyte trafficking to the lungs and beyond: lessons from influenza for COVID-19. Nat Rev Immunol 2021;21:49–64. https://doi.org/10.1038/s41577-020-00470-2."
},
{
"DOI": "10.1007/978-3-030-53868-2_5",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_018",
"unstructured": "Land, WG. DAMP-promoted efferent innate immune responses in human diseases: inflammation. In: Land, WG, editor Damage-associated molecular patterns in human diseases: volume 2: danger signals as diagnostics, prognostics, and therapeutic targets. Cham: Springer International Publishing; 2020:151–209 pp."
},
{
"DOI": "10.1007/s40266-014-0178-0",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_019",
"unstructured": "Vural, EM, van Munster, BC, de Rooij, SE. Optimal dosages for melatonin supplementation therapy in older adults: a systematic review of current literature. Drugs Aging 2014;31:441–51. https://doi.org/10.1007/s40266-014-0178-0."
},
{
"DOI": "10.1155/2020/6286105",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_020",
"unstructured": "Perez-Garmendia, R, Lopez de Eguileta Rodriguez, A, Ramos-Martinez, I, Zuñiga, NM, Gonzalez-Salinas, R, Quiroz-Mercado, H, et al.. Interplay between oxidative stress, inflammation, and amyloidosis in the anterior segment of the eye; its pathological implications. Oxid Med Cell Longev 2020;2020:6286105. https://doi.org/10.1155/2020/6286105."
},
{
"DOI": "10.1089/ars.2020.8124",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_021",
"unstructured": "Amaral, EP, Vinhaes, CL, Oliveira-de-Souza, D, Nogueira, B, Akrami, KM, Andrade, BB. The interplay between systemic inflammation, oxidative stress, and tissue remodeling in tuberculosis. Antioxidants Redox Signal 2021;34:471–85. https://doi.org/10.1089/ars.2020.8124."
},
{
"DOI": "10.3390/antiox9100936",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_022",
"unstructured": "Beltrán-García, J, Osca-Verdegal, R, Pallardó, FV, Ferreres, J, Rodríguez, M, Mulet, S, et al.. Oxidative stress and inflammation in COVID-19-associated sepsis: the potential role of anti-oxidant therapy in avoiding disease progression. Antioxidants 2020;9. https://doi.org/10.3390/antiox9100936."
},
{
"DOI": "10.1080/08830185.2020.1845330",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_023",
"unstructured": "Arjunan, P. Eye on the enigmatic link: dysbiotic oral pathogens in ocular diseases; the flip side. Int Rev Immunol 2020:1–24. https://doi.org/10.1080/08830185.2020.1845330."
},
{
"DOI": "10.1371/journal.pone.0178525",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_024",
"unstructured": "Yu, GM, Kubota, H, Okita, M, Maeda, T. The anti-inflammatory and antioxidant effects of melatonin on LPS-stimulated bovine mammary epithelial cells. PLoS One 2017;12:e0178525. https://doi.org/10.1371/journal.pone.0178525."
},
{
"DOI": "10.1111/j.1600-079X.2008.00560.x",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_025",
"unstructured": "Huang, SH, Cao, XJ, Wei, W. Melatonin decreases TLR3-mediated inflammatory factor expression via inhibition of NF-kappa B activation in respiratory syncytial virus-infected RAW264.7 macrophages. J Pineal Res 2008;45:93–100. https://doi.org/10.1111/j.1600-079x.2008.00560.x."
},
{
"DOI": "10.1111/j.1600-079X.2009.00733.x",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_026",
"unstructured": "Huang, SH, Cao, XJ, Liu, W, Shi, XY, Wei, W. Inhibitory effect of melatonin on lung oxidative stress induced by respiratory syncytial virus infection in mice. J Pineal Res 2010;48:109–16. https://doi.org/10.1111/j.1600-079x.2009.00733.x."
},
{
"key": "2023040103062794722_j_znc-2021-0101_ref_027",
"unstructured": "Ueda, K, Park, JH, Ochiai, K, Itakura, C. Disseminated intravascular coagulation (DIC) in rabbit haemorrhagic disease. Jpn J Vet Res 1992;40:133–41."
},
{
"DOI": "10.1002/ejhf.665",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_028",
"unstructured": "Verdonschot, J, Hazebroek, M, Merken, J, Debing, Y, Dennert, R, Brunner-La Rocca, HP, et al.. Relevance of cardiac parvovirus B19 in myocarditis and dilated cardiomyopathy: review of the literature. Eur J Heart Fail 2016;18:1430–41. https://doi.org/10.1002/ejhf.665."
},
{
"DOI": "10.1007/s10735-019-09836-w",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_029",
"unstructured": "Ouyang, H, Zhong, J, Lu, J, Zhong, Y, Hu, Y, Tan, Y. Inhibitory effect of melatonin on Mst1 ameliorates myocarditis through attenuating ER stress and mitochondrial dysfunction. J Mol Histol 2019;50:405–15. https://doi.org/10.1007/s10735-019-09836-w."
},
{
"DOI": "10.1111/jpi.12322",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_030",
"unstructured": "Zhang, Y, Li, X, Grailer, JJ, Wang, N, Wang, M, Yao, J, et al.. Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J Pineal Res 2016;60:405–14. https://doi.org/10.1111/jpi.12322."
},
{
"DOI": "10.1155/2017/1835195",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_031",
"unstructured": "Favero, G, Franceschetti, L, Bonomini, F, Rodella, LF, Rezzani, R. Melatonin as an anti-inflammatory agent modulating inflammasome activation. Internet J Endocrinol 2017;2017:1835195. https://doi.org/10.1155/2017/1835195."
},
{
"DOI": "10.1111/jpi.12414",
"doi-asserted-by": "crossref",
"key": "2023040103062794722_j_znc-2021-0101_ref_032",
"unstructured": "Liu, Z, Gan, L, Xu, Y, Luo, D, Ren, Q, Wu, S, et al.. Melatonin alleviates inflammasome-induced pyroptosis through inhibiting NF-κB/GSDMD signal in mice adipose tissue. J Pineal Res 2017;63. https://doi.org/10.1111/jpi.12414."
}
],
"reference-count": 32,
"references-count": 32,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.degruyter.com/document/doi/10.1515/znc-2021-0101/html"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "NLRP3 inflammasome activation and oxidative stress status in the mild and moderate SARS-CoV-2 infected patients: impact of melatonin as a medicinal supplement",
"type": "journal-article",
"volume": "77"
}