Central nervous system and systemic inflammatory networks associated with acute neurological outcomes in COVID-19
et al., Scientific Reports, doi:10.1038/s41598-025-08632-9, Jul 2025
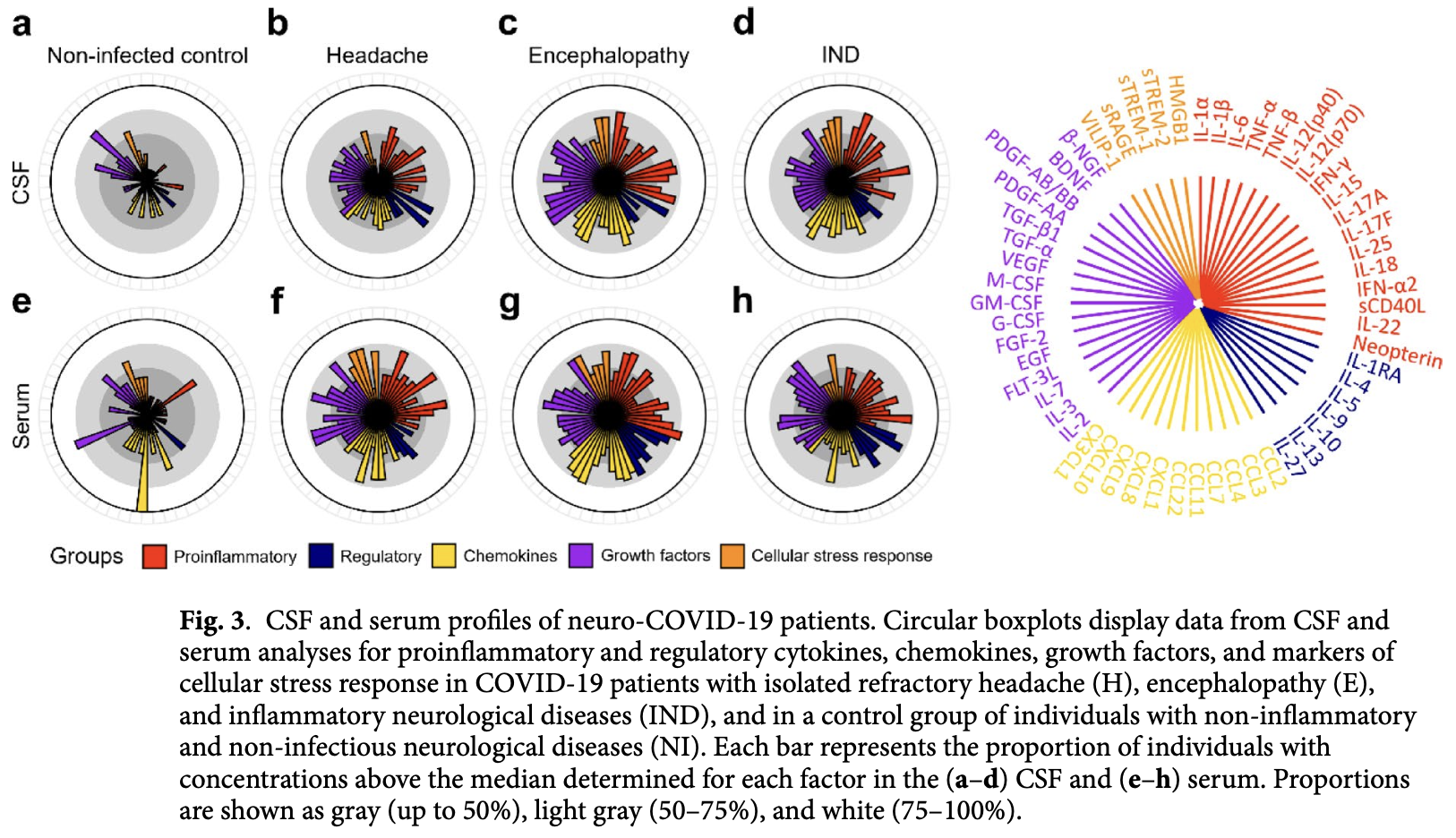
Analysis of 52 COVID-19 patients with neurological manifestations, showing distinct inflammatory profiles in cerebrospinal fluid (CSF) and serum associated with different neurological outcomes. Patients were categorized into three groups: isolated refractory headache (n=14), encephalopathy (n=24), and inflammatory neurological diseases (IND) (n=14). All COVID-19 patients exhibited elevated CSF levels of proinflammatory mediators, with patients with encephalopathy and IND showing more extensive CNS inflammation consistent with cytokine storm. Patients with isolated refractory headache showed a more modest inflammatory profile. The study suggests that both systemic immune activation and localized neuroinflammation contribute to the diversity of neurological outcomes observed in COVID-19, with dysregulated cytokine production, glial activation, inflammasome activity, and blood-brain barrier disturbances representing key factors in neuro-COVID-19 pathogenesis.
Freitas et al., 6 Jul 2025, peer-reviewed, 9 authors.
Contact: otavio.espindola@ini.fiocruz.br.
Central nervous system and systemic inflammatory networks associated with acute neurological outcomes in COVID-19
Scientific Reports, doi:10.1038/s41598-025-08632-9
COVID-19 is associated with a wide spectrum of neurological alterations, ranging from headache and dizziness to severe encephalopathy and inflammatory neurological diseases (IND), and neuropathological findings suggest immune-mediated processes. Therefore, we sought to characterize profiles of cytokines, chemokines, growth factors, and markers of central nervous system (CNS) homeostasis in COVID-19 patients with neurological alterations to identify key factors and mechanisms underlying CNS disturbances in COVID-19. The study included a case series of 52 COVID-19 patients with neurological manifestations, which were categorized into three groups: isolated refractory headache (n = 14), encephalopathy (n = 24), and IND (n = 14). Individuals with non-inflammatory, noninfectious neurological conditions (n = 9) were included as negative controls. Paired CSF and serum samples were assessed for 56 biomarkers. Regardless of the neurological condition, COVID-19 patients exhibited elevated CSF levels of proinflammatory mediators, including IL-2, IL-3, IL-6, IL-15, IL-25, IFN-α2, CCL7, CCL11, and GM-CSF. Patients with encephalopathy and IND also showed increased IL-1β, IL-18, TNF-α, neopterin, IL-7, CXCL8, CXCL9, TGF-α, EGF, sTREM-2, and HMGB1, consistent with a CNS cytokine storm. In contrast, individuals with isolated refractory headache showed a modest inflammatory profile, compatible with the limited CNS involvement. COVID-19 patients showed elevated serum IL-13, IL-18, TNF-α, VILIP-1, TGF-α, and VEGF levels, indicating systemic inflammation and potential blood-brain barrier (BBB) disruption. β-NGF was increased in the CSF of patients with encephalopathy and IND, suggesting the activation of neuroprotective responses during patient recovery. Functional protein network analysis showed a significant enrichment of interactions between factors altered in the CSF of patients with encephalopathy and IND, many of them related to processes of neuroinflammation and microglial functions, and leukocyte chemotaxis, activation and proliferation. These findings support a model in which both systemic immune activation and localized neuroinflammation contribute to the diversity of neurological outcomes observed in COVID-19, and dysregulated cytokine production, glial activation, inflammasome activity and BBB disturbances represent key factors in neuro-COVID-19 pathogenesis. At the onset of the Coronavirus Disease 2019 (COVID-19) pandemic, many groups reported the involvement of the central and peripheral nervous systems in SARS-CoV-2 infection. Patients displayed neurological manifestations as the initial presentation or after the onset of classic symptoms such as fever, cough, diarrhea, and fatigue 1-6 . Central nervous system (CNS) manifestations, including headache, dizziness, altered consciousness, and acute cerebrovascular disease, were more common in severe cases than in patients with mild to moderate symptoms as determined by their respiratory status 5 . In..
Author contributions N.L.F. performed cytometry bead-based multiplex assays with assistance from R.C.T., conducted ELISA, data analysis, and drafted the manuscript; J.V.C.D. carried out functional network analysis; K.S., performed Luminex assays; Y.C.P.G. performed data analysis; C.O.B. performed CSF and paired serum laboratory analysis; C.N.S. and M.T.T.S. acquired clinical data and conducted neurological assessments; N.F.L., J.V.C.D., and O.M.E assembled the figures; O.M.E. and M.T.T.S contributed to the study concept and design; O.M.E performed data analysis, supervised all phases of the project, and drafted the manuscript. All authors contributed to interpretation of the results, read and approved the final manuscript.
Declarations
Competing interests The authors declare no competing interests.
Ethics approval and consent to participate The study protocol was approved by the Brazilian National Committee of Ethics in Research on April 22, 2020 (Protocol number CAAE 30611720.6.0000.5262), and written informed consent was obtained from all participants. All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Supplementary Information The online version contains supplementary material available at h t t p s : / / d o i . o r g / 1 0 . 1 0 3 8 / s 4 1 5 9 8 -0 2 5 -0 8 6 3 2 -9 . Correspondence and requests for materials should be addressed to O.M.E. Reprints and permissions information is available at ..
References
Aloe, Rocco, Bianchi, Manni, Nerve growth factor: From the early discoveries to the potential clinical use, J. Transl. Med
Azim, Nasim, Kumar, Hussain, Patel, Neurological consequences of 2019-nCoV infection: A comprehensive literature review, Cureus
Azoulay, Recovery from SARS-CoV-2 infection is associated with serum BDNF restoration, J. Infect
Azoulay, Urshansky, Karni, Low and dysregulated BDNF secretion from immune cells of MS patients is related to reduced neuroprotection, J. Neuroimmunol
Ceban, COVID-19 vaccination for the prevention and treatment of long COVID: A systematic review and meta-analysis, Brain Behav. Immun
Chang, Neurological disorders associated with COVID-19 in Sri Lanka, BMC Neurol
Chaumont, Cerebrospinal fluid biomarkers in SARS-CoV-2 patients with acute neurological syndromes, Rev. Neurol
Chen, Prior COVID-19 vaccination and reduced risk of cerebrovascular diseases among COVID-19 survivors, J. Med. Virol
De Espíndola, Patients with COVID-19 and neurological manifestations show undetectable SARS-CoV-2 RNA levels in the cerebrospinal fluid, Int. J. Infect. Dis
De Paula Martins, Neopterin preconditioning prevents inflammasome activation in mammalian astrocytes, Free Radic. Biol. Med
Edén, Viral antigen and inflammatory biomarkers in cerebrospinal fluid in patients With COVID-19 infection and neurologic symptoms compared with control participants without infection or neurologic symptoms, JAMA Netw. Open
Eisenhut, Neopterin in diagnosis and monitoring of infectious diseases, J. Biomark
Ellul, Neurological associations of COVID-19, Lancet Neurol
Espíndola, Cerebrospinal fluid findings in neurological diseases associated with COVID-19 and insights into mechanisms of disease development, Int. J. Infect. Dis
Espíndola, Inflammatory cytokine patterns Associated with neurological diseases in coronavirus disease 2019, Ann. Neurol
Fan, SARS-CoV-2 Omicron variant: Recent progress and future perspectives, Signal Transduct. Target Ther
Fernández-De-Las-Peñas, Long-COVID symptoms in individuals infected with different SARS-CoV-2 variants of concern: A systematic review of the literature, Viruses
Garg, Paliwal, Gupta, Encephalopathy in patients with COVID-19: A review, J. Med. Virol. h t t, doi:10.1002/jmv.26207
Gavard, Gutkind, VEGF controls endothelial-cell permeability by promoting the beta-arrestin-dependent endocytosis of VE-cadherin, Nat. Cell Biol
Ghisoni, De Martins, Barbeito, Latini, Neopterin as a potential cytoprotective brain molecule, J. Psychiatr. Res
Gierke, Expression analysis of members of the neuronal calcium sensor protein family: Combining bioinformatics and Western blot analysis, Biochem. Biophys. Res. Commun
Gong, Clinical and immunological features in patients with neuroimmune complications of COVID-19 during Omicron wave in China: A case series, Front. Immunol
Gupta, Extrapulmonary manifestations of COVID-19, Nat. Med
Halbgebauer, Visinin-like protein 1 levels in blood and CSF as emerging markers for Alzheimer's and other neurodegenerative diseases, Alzheimers Res. Ther
Helms, Neurologic features in severe SARS-CoV-2 infection, N. Engl. J. Med
Hoffmann, Wirleitner, Fuchs, Potential role of immune system activation-associated production of neopterin derivatives in humans, Inflamm. Res
Jardim-Santos, Unbalanced networks and disturbed kinetics of serum soluble mediators associated with distinct disease outcomes in severe COVID-19 patients, Front Immunol
Kleinschek, IL-25 regulates Th17 function in autoimmune inflammation, J. Exp. Med
Lavi, Cong, Type I astrocytes and microglia induce a cytokine response in an encephalitic murine coronavirus infection, Exp. Mol. Pathol
Liu, Immune-boosting effect of the COVID-19 vaccine: Real-world bidirectional cohort study, JMIR Public Health Surveill
Lotfi, Roles of GM-CSF in the pathogenesis of autoimmune diseases: An update, Front. Immunol
Lu, Neurological complications during the omicron COVID-19 wave in China: A cohort study, Eur. J. Neurol
Luo, Chu, Zhang, Xia, Chen, Fractalkine/CX3CR1 is involved in the cross-talk between neuron and glia in neurological diseases, Brain Res. Bull
Mao, Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China, JAMA Neurol, doi:10.1001/jamaneurol.2020.1127
Pezzini, Padovani, Lifting the mask on neurological manifestations of COVID-19, Nat. Rev. Neurol
Pilotto, Steroid-responsive encephalitis in coronavirus disease 2019, Ann. Neurol, doi:10.1002/ana.25783
Puelles, Multiorgan and renal tropism of SARS-CoV-2, N. Engl. J. Med
Rabchevsky, A role for transforming growth factor alpha as an inducer of astrogliosis, J. Neurosci
Ren, Zhao, Sun, Wang, Shi, HMGB1 and Toll-like receptors: Potential therapeutic targets in autoimmune diseases, Mol. Med
Savarin, Bergmann, Fine tuning the cytokine storm by IFN and IL-10 following neurotropic coronavirus encephalomyelitis, Front. Immunol
Schnurra, Bernstein, Riederer, Braunewell, The neuronal calcium sensor protein VILIP-1 is associated with amyloid plaques and extracellular tangles in Alzheimer's disease and promotes cell death and tau phosphorylation in vitro: A link between calcium sensors and Alzheimer's disease?, Neurobiol. Dis
Sha, Chen, Infection routes, invasion mechanisms, and drug inhibition pathways of human coronaviruses on the nervous system, Front. Neurosci
Silva, Isolated intracranial hypertension associated with COVID-19, Cephalalgia
Sobczak, Pawliczak, COVID-19 vaccination efficacy in numbers including SARS-CoV-2 variants and age comparison: A meta-analysis of randomized clinical trials, Ann. Clin. Microbiol. Antimicrob
Solomon, Neuropathological features of Covid-19, N. Engl. J. Med
Sonobe, Interleukin-25 expressed by brain capillary endothelial cells maintains blood-brain barrier function in a protein kinase Cepsilon-dependent manner, J. Biol. Chem
Steele, Estimated Number of COVID-19 infections, hospitalizations, and deaths prevented among vaccinated persons in the US, December 2020 to, JAMA Netw. Open
Thaweethai, Development of a definition of postacute sequelae of SARS-CoV-2 infection, JAMA
Vande Walle, Kanneganti, Lamkanfi, HMGB1 release by inflammasomes, Virulence
Vargas, Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and glial cells: Insights and perspectives, Brain, Behav. Immun. Health
Venkatesan, Case definitions, diagnostic algorithms, and priorities in encephalitis: Consensus statement of the international encephalitis consortium, Clin. Infect. Dis
Viaccoz, CSF neopterin level as a diagnostic marker in primary central nervous system lymphoma, Neuro Oncol
Wang, Dentler, Borchardt, VEGF increases BMEC monolayer permeability by affecting occludin expression and tight junction assembly, Am. J. Physiol. Heart Circ. Physiol
Wong, Guillaud, The role of epidermal growth factor and its receptors in mammalian CNS, Cytokine Growth Fact. Rev
Yang, Wang, Andersson, Targeting inflammation driven by HMGB1, Front. Immunol
Zhu, Dynamics of inflammatory responses after SARS-CoV-2 infection by vaccination status in the USA: A prospective cohort study, Lancet Microbe
DOI record:
{
"DOI": "10.1038/s41598-025-08632-9",
"ISSN": [
"2045-2322"
],
"URL": "http://dx.doi.org/10.1038/s41598-025-08632-9",
"alternative-id": [
"8632"
],
"article-number": "24154",
"assertion": [
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Received",
"name": "received",
"order": 1,
"value": "11 March 2025"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "23 June 2025"
},
{
"group": {
"label": "Article History",
"name": "ArticleHistory"
},
"label": "First Online",
"name": "first_online",
"order": 3,
"value": "6 July 2025"
},
{
"group": {
"label": "Declarations",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 1
},
{
"group": {
"label": "Competing interests",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 2,
"value": "The authors declare no competing interests."
},
{
"group": {
"label": "Ethics approval and consent to participate",
"name": "EthicsHeading"
},
"name": "Ethics",
"order": 3,
"value": "The study protocol was approved by the Brazilian National Committee of Ethics in Research on April 22, 2020 (Protocol number CAAE 30611720.6.0000.5262), and written informed consent was obtained from all participants. All methods were performed in accordance with the relevant guidelines and regulations."
}
],
"author": [
{
"affiliation": [],
"family": "Freitas",
"given": "Nicole Lardini",
"sequence": "first"
},
{
"affiliation": [],
"family": "Deus",
"given": "João Victor Carvalho",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sampaio",
"given": "Karen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gomes",
"given": "Yago Côrtes Pinheiro",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Torres",
"given": "Rafael Carvalho",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Brandão",
"given": "Carlos Otávio",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Soares",
"given": "Cristiane Nascimento",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Silva",
"given": "Marcus Tulius Teixeira",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Espíndola",
"given": "Otávio Melo",
"sequence": "additional"
}
],
"container-title": "Scientific Reports",
"container-title-short": "Sci Rep",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"link.springer.com"
]
},
"created": {
"date-parts": [
[
2025,
7,
6
]
],
"date-time": "2025-07-06T16:58:18Z",
"timestamp": 1751821098000
},
"deposited": {
"date-parts": [
[
2025,
7,
6
]
],
"date-time": "2025-07-06T18:02:58Z",
"timestamp": 1751824978000
},
"funder": [
{
"award": [
"Finance code 001"
],
"name": "Coordination of Superior Level Staff Improvement"
},
{
"name": "Brazilian National Council for Scientific and Technological Development"
},
{
"DOI": "10.13039/501100006507",
"award": [
"VPPCB-005-FIO-20-2-65"
],
"doi-asserted-by": "crossref",
"id": [
{
"asserted-by": "crossref",
"id": "10.13039/501100006507",
"id-type": "DOI"
}
],
"name": "Fundação Oswaldo Cruz"
},
{
"award": [
"E-26/200.157/2023"
],
"name": "Carlos Chagas Foundation for the Advancement of Science of the State of Rio de Janeiro"
}
],
"indexed": {
"date-parts": [
[
2025,
7,
6
]
],
"date-time": "2025-07-06T18:40:08Z",
"timestamp": 1751827208459,
"version": "3.41.0"
},
"is-referenced-by-count": 0,
"issue": "1",
"issued": {
"date-parts": [
[
2025,
7,
6
]
]
},
"journal-issue": {
"issue": "1",
"published-online": {
"date-parts": [
[
2025,
12
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
7,
6
]
],
"date-time": "2025-07-06T00:00:00Z",
"timestamp": 1751760000000
}
},
{
"URL": "https://creativecommons.org/licenses/by-nc-nd/4.0",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2025,
7,
6
]
],
"date-time": "2025-07-06T00:00:00Z",
"timestamp": 1751760000000
}
}
],
"link": [
{
"URL": "https://www.nature.com/articles/s41598-025-08632-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-025-08632-9",
"content-type": "text/html",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.nature.com/articles/s41598-025-08632-9.pdf",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "297",
"original-title": [],
"prefix": "10.1038",
"published": {
"date-parts": [
[
2025,
7,
6
]
]
},
"published-online": {
"date-parts": [
[
2025,
7,
6
]
]
},
"publisher": "Springer Science and Business Media LLC",
"reference": [
{
"author": "D Azim",
"first-page": "e8790",
"journal-title": "Cureus",
"key": "8632_CR1",
"unstructured": "Azim, D., Nasim, S., Kumar, S., Hussain, A. & Patel, S. Neurological consequences of 2019-nCoV infection: A comprehensive literature review. Cureus 12, e8790 (2020).",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1016/S1474-4422(20)30221-0",
"author": "MA Ellul",
"doi-asserted-by": "publisher",
"first-page": "767",
"journal-title": "Lancet Neurol.",
"key": "8632_CR2",
"unstructured": "Ellul, M. A. et al. Neurological associations of COVID-19. Lancet Neurol. 19, 767–783 (2020).",
"volume": "19",
"year": "2020"
},
{
"DOI": "10.1002/jmv.26207",
"author": "RK Garg",
"doi-asserted-by": "publisher",
"journal-title": "J. Med. Virol.",
"key": "8632_CR3",
"unstructured": "Garg, R. K., Paliwal, V. K. & Gupta, A. Encephalopathy in patients with COVID-19: A review. J. Med. Virol. https://doi.org/10.1002/jmv.26207 (2020).",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2008597",
"author": "J Helms",
"doi-asserted-by": "publisher",
"first-page": "2268",
"journal-title": "N. Engl. J. Med.",
"key": "8632_CR4",
"unstructured": "Helms, J. et al. Neurologic features in severe SARS-CoV-2 infection. N. Engl. J. Med. 382, 2268–2270 (2020).",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1001/jamaneurol.2020.1127",
"author": "L Mao",
"doi-asserted-by": "publisher",
"journal-title": "JAMA Neurol.",
"key": "8632_CR5",
"unstructured": "Mao, L. et al. Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol. https://doi.org/10.1001/jamaneurol.2020.1127 (2020).",
"year": "2020"
},
{
"DOI": "10.1016/j.ijid.2020.10.044",
"author": "OM Espíndola",
"doi-asserted-by": "publisher",
"first-page": "155",
"journal-title": "Int. J. Infect. Dis.",
"key": "8632_CR6",
"unstructured": "Espíndola, O. M. et al. Cerebrospinal fluid findings in neurological diseases associated with COVID-19 and insights into mechanisms of disease development. Int. J. Infect. Dis. 102, 155–162 (2021).",
"volume": "102",
"year": "2021"
},
{
"DOI": "10.1186/s12941-022-00525-3",
"author": "M Sobczak",
"doi-asserted-by": "publisher",
"first-page": "32",
"journal-title": "Ann. Clin. Microbiol. Antimicrob.",
"key": "8632_CR7",
"unstructured": "Sobczak, M. & Pawliczak, R. COVID-19 vaccination efficacy in numbers including SARS-CoV-2 variants and age comparison: A meta-analysis of randomized clinical trials. Ann. Clin. Microbiol. Antimicrob. 21, 32 (2022).",
"volume": "21",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2022.20385",
"author": "MK Steele",
"doi-asserted-by": "publisher",
"first-page": "e2220385",
"journal-title": "JAMA Netw. Open",
"key": "8632_CR8",
"unstructured": "Steele, M. K. et al. Estimated Number of COVID-19 infections, hospitalizations, and deaths prevented among vaccinated persons in the US, December 2020 to September 2021. JAMA Netw. Open 5, e2220385 (2022).",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.1001/jama.2023.8823",
"author": "T Thaweethai",
"doi-asserted-by": "publisher",
"first-page": "1934",
"journal-title": "JAMA",
"key": "8632_CR9",
"unstructured": "Thaweethai, T. et al. Development of a definition of postacute sequelae of SARS-CoV-2 infection. JAMA 329, 1934–1946 (2023).",
"volume": "329",
"year": "2023"
},
{
"DOI": "10.1016/j.bbih.2020.100127",
"author": "G Vargas",
"doi-asserted-by": "publisher",
"first-page": "100127",
"journal-title": "Brain, Behav. Immun. Health",
"key": "8632_CR10",
"unstructured": "Vargas, G. et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and glial cells: Insights and perspectives. Brain, Behav. Immun. Health 7, 100127 (2020).",
"volume": "7",
"year": "2020"
},
{
"DOI": "10.3389/fnins.2023.1169740",
"author": "A Sha",
"doi-asserted-by": "publisher",
"first-page": "1169740",
"journal-title": "Front. Neurosci.",
"key": "8632_CR11",
"unstructured": "Sha, A. & Chen, H. Infection routes, invasion mechanisms, and drug inhibition pathways of human coronaviruses on the nervous system. Front. Neurosci. 17, 1169740 (2023).",
"volume": "17",
"year": "2023"
},
{
"DOI": "10.1038/s41582-020-0398-3",
"author": "A Pezzini",
"doi-asserted-by": "publisher",
"first-page": "636",
"journal-title": "Nat. Rev. Neurol.",
"key": "8632_CR12",
"unstructured": "Pezzini, A. & Padovani, A. Lifting the mask on neurological manifestations of COVID-19. Nat. Rev. Neurol. 16, 636–644 (2020).",
"volume": "16",
"year": "2020"
},
{
"DOI": "10.3390/v14122629",
"author": "C Fernández-de-Las-Peñas",
"doi-asserted-by": "publisher",
"first-page": "2629",
"journal-title": "Viruses",
"key": "8632_CR13",
"unstructured": "Fernández-de-Las-Peñas, C. et al. Long-COVID symptoms in individuals infected with different SARS-CoV-2 variants of concern: A systematic review of the literature. Viruses 14, 2629 (2022).",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1002/ana.26041",
"author": "OM Espíndola",
"doi-asserted-by": "publisher",
"first-page": "1041",
"journal-title": "Ann. Neurol.",
"key": "8632_CR14",
"unstructured": "Espíndola, O. M. et al. Inflammatory cytokine patterns Associated with neurological diseases in coronavirus disease 2019. Ann. Neurol. 89, 1041–1045 (2021).",
"volume": "89",
"year": "2021"
},
{
"DOI": "10.1177/0333102420965963",
"author": "MTT Silva",
"doi-asserted-by": "publisher",
"first-page": "1452",
"journal-title": "Cephalalgia",
"key": "8632_CR15",
"unstructured": "Silva, M. T. T. et al. Isolated intracranial hypertension associated with COVID-19. Cephalalgia 40, 1452–1458 (2020).",
"volume": "40",
"year": "2020"
},
{
"DOI": "10.1093/cid/cit458",
"author": "A Venkatesan",
"doi-asserted-by": "publisher",
"first-page": "1114",
"journal-title": "Clin. Infect. Dis.",
"key": "8632_CR16",
"unstructured": "Venkatesan, A. et al. Case definitions, diagnostic algorithms, and priorities in encephalitis: Consensus statement of the international encephalitis consortium. Clin. Infect. Dis. 57, 1114–1128 (2013).",
"volume": "57",
"year": "2013"
},
{
"DOI": "10.3389/fimmu.2022.1004023",
"author": "GP Jardim-Santos",
"doi-asserted-by": "publisher",
"first-page": "1004023",
"journal-title": "Front Immunol",
"key": "8632_CR17",
"unstructured": "Jardim-Santos, G. P. et al. Unbalanced networks and disturbed kinetics of serum soluble mediators associated with distinct disease outcomes in severe COVID-19 patients. Front Immunol 13, 1004023 (2022).",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.ijid.2020.05.123",
"author": "OM de Espíndola",
"doi-asserted-by": "publisher",
"first-page": "567",
"journal-title": "Int. J. Infect. Dis.",
"key": "8632_CR18",
"unstructured": "de Espíndola, O. M. et al. Patients with COVID-19 and neurological manifestations show undetectable SARS-CoV-2 RNA levels in the cerebrospinal fluid. Int. J. Infect. Dis. 96, 567–569 (2020).",
"volume": "96",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2011400",
"author": "VG Puelles",
"doi-asserted-by": "publisher",
"first-page": "590",
"journal-title": "N. Engl. J. Med.",
"key": "8632_CR19",
"unstructured": "Puelles, V. G. et al. Multiorgan and renal tropism of SARS-CoV-2. N. Engl. J. Med. 383, 590–592 (2020).",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1056/NEJMc2019373",
"author": "IH Solomon",
"doi-asserted-by": "publisher",
"first-page": "989",
"journal-title": "N. Engl. J. Med.",
"key": "8632_CR20",
"unstructured": "Solomon, I. H. et al. Neuropathological features of Covid-19. N. Engl. J. Med. 383, 989–992 (2020).",
"volume": "383",
"year": "2020"
},
{
"DOI": "10.1002/ana.25783",
"author": "A Pilotto",
"doi-asserted-by": "publisher",
"journal-title": "Ann. Neurol.",
"key": "8632_CR21",
"unstructured": "Pilotto, A. et al. Steroid-responsive encephalitis in coronavirus disease 2019. Ann. Neurol. https://doi.org/10.1002/ana.25783 (2020).",
"year": "2020"
},
{
"DOI": "10.1016/j.brainresbull.2018.11.017",
"author": "P Luo",
"doi-asserted-by": "publisher",
"first-page": "12",
"journal-title": "Brain Res. Bull.",
"key": "8632_CR22",
"unstructured": "Luo, P., Chu, S.-F., Zhang, Z., Xia, C.-Y. & Chen, N.-H. Fractalkine/CX3CR1 is involved in the cross-talk between neuron and glia in neurological diseases. Brain Res. Bull. 146, 12–21 (2019).",
"volume": "146",
"year": "2019"
},
{
"DOI": "10.1523/JNEUROSCI.18-24-10541.1998",
"author": "AG Rabchevsky",
"doi-asserted-by": "publisher",
"first-page": "10541",
"journal-title": "J. Neurosci.",
"key": "8632_CR23",
"unstructured": "Rabchevsky, A. G. et al. A role for transforming growth factor alpha as an inducer of astrogliosis. J. Neurosci. 18, 10541–10552 (1998).",
"volume": "18",
"year": "1998"
},
{
"DOI": "10.1006/nbdi.2001.0432",
"author": "I Schnurra",
"doi-asserted-by": "publisher",
"first-page": "900",
"journal-title": "Neurobiol. Dis.",
"key": "8632_CR24",
"unstructured": "Schnurra, I., Bernstein, H. G., Riederer, P. & Braunewell, K. H. The neuronal calcium sensor protein VILIP-1 is associated with amyloid plaques and extracellular tangles in Alzheimer’s disease and promotes cell death and tau phosphorylation in vitro: A link between calcium sensors and Alzheimer’s disease?. Neurobiol. Dis. 8, 900–909 (2001).",
"volume": "8",
"year": "2001"
},
{
"DOI": "10.1186/s13195-022-01122-4",
"author": "S Halbgebauer",
"doi-asserted-by": "publisher",
"first-page": "175",
"journal-title": "Alzheimers Res. Ther.",
"key": "8632_CR25",
"unstructured": "Halbgebauer, S. et al. Visinin-like protein 1 levels in blood and CSF as emerging markers for Alzheimer’s and other neurodegenerative diseases. Alzheimers Res. Ther. 14, 175 (2022).",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.1016/j.bbrc.2004.08.055",
"author": "P Gierke",
"doi-asserted-by": "publisher",
"first-page": "38",
"journal-title": "Biochem. Biophys. Res. Commun.",
"key": "8632_CR26",
"unstructured": "Gierke, P. et al. Expression analysis of members of the neuronal calcium sensor protein family: Combining bioinformatics and Western blot analysis. Biochem. Biophys. Res. Commun. 323, 38–43 (2004).",
"volume": "323",
"year": "2004"
},
{
"DOI": "10.1016/j.jneuroim.2008.01.010",
"author": "D Azoulay",
"doi-asserted-by": "publisher",
"first-page": "186",
"journal-title": "J. Neuroimmunol.",
"key": "8632_CR27",
"unstructured": "Azoulay, D., Urshansky, N. & Karni, A. Low and dysregulated BDNF secretion from immune cells of MS patients is related to reduced neuroprotection. J. Neuroimmunol. 195, 186–193 (2008).",
"volume": "195",
"year": "2008"
},
{
"DOI": "10.1016/j.jinf.2020.06.038",
"author": "D Azoulay",
"doi-asserted-by": "publisher",
"first-page": "e79",
"journal-title": "J. Infect.",
"key": "8632_CR28",
"unstructured": "Azoulay, D. et al. Recovery from SARS-CoV-2 infection is associated with serum BDNF restoration. J. Infect. 81, e79–e81 (2020).",
"volume": "81",
"year": "2020"
},
{
"DOI": "10.1152/ajpheart.2001.280.1.H434",
"author": "W Wang",
"doi-asserted-by": "publisher",
"first-page": "H434",
"journal-title": "Am. J. Physiol. Heart Circ. Physiol.",
"key": "8632_CR29",
"unstructured": "Wang, W., Dentler, W. L. & Borchardt, R. T. VEGF increases BMEC monolayer permeability by affecting occludin expression and tight junction assembly. Am. J. Physiol. Heart Circ. Physiol. 280, H434-440 (2001).",
"volume": "280",
"year": "2001"
},
{
"DOI": "10.1038/ncb1486",
"author": "J Gavard",
"doi-asserted-by": "publisher",
"first-page": "1223",
"journal-title": "Nat. Cell Biol.",
"key": "8632_CR30",
"unstructured": "Gavard, J. & Gutkind, J. S. VEGF controls endothelial-cell permeability by promoting the beta-arrestin-dependent endocytosis of VE-cadherin. Nat. Cell Biol. 8, 1223–1234 (2006).",
"volume": "8",
"year": "2006"
},
{
"DOI": "10.3389/fimmu.2019.01265",
"author": "N Lotfi",
"doi-asserted-by": "publisher",
"first-page": "1265",
"journal-title": "Front. Immunol.",
"key": "8632_CR31",
"unstructured": "Lotfi, N. et al. Roles of GM-CSF in the pathogenesis of autoimmune diseases: An update. Front. Immunol. 10, 1265 (2019).",
"volume": "10",
"year": "2019"
},
{
"DOI": "10.1001/jamanetworkopen.2022.13253",
"author": "A Edén",
"doi-asserted-by": "publisher",
"first-page": "e2213253",
"journal-title": "JAMA Netw. Open",
"key": "8632_CR32",
"unstructured": "Edén, A. et al. Viral antigen and inflammatory biomarkers in cerebrospinal fluid in patients With COVID-19 infection and neurologic symptoms compared with control participants without infection or neurologic symptoms. JAMA Netw. Open 5, e2213253 (2022).",
"volume": "5",
"year": "2022"
},
{
"DOI": "10.1016/j.neurol.2022.11.002",
"author": "H Chaumont",
"doi-asserted-by": "publisher",
"first-page": "208",
"journal-title": "Rev. Neurol. (Paris)",
"key": "8632_CR33",
"unstructured": "Chaumont, H. et al. Cerebrospinal fluid biomarkers in SARS-CoV-2 patients with acute neurological syndromes. Rev. Neurol. (Paris) 179, 208–217 (2023).",
"volume": "179",
"year": "2023"
},
{
"DOI": "10.1007/s00011-003-1181-9",
"author": "G Hoffmann",
"doi-asserted-by": "publisher",
"first-page": "313",
"journal-title": "Inflamm. Res.",
"key": "8632_CR34",
"unstructured": "Hoffmann, G., Wirleitner, B. & Fuchs, D. Potential role of immune system activation-associated production of neopterin derivatives in humans. Inflamm. Res. 52, 313–321 (2003).",
"volume": "52",
"year": "2003"
},
{
"DOI": "10.1155/2013/196432",
"author": "M Eisenhut",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J. Biomark.",
"key": "8632_CR35",
"unstructured": "Eisenhut, M. Neopterin in diagnosis and monitoring of infectious diseases. J. Biomark. 2013, 1–10 (2013).",
"volume": "2013",
"year": "2013"
},
{
"DOI": "10.1093/neuonc/nov092",
"author": "A Viaccoz",
"doi-asserted-by": "publisher",
"first-page": "1497",
"journal-title": "Neuro Oncol.",
"key": "8632_CR36",
"unstructured": "Viaccoz, A. et al. CSF neopterin level as a diagnostic marker in primary central nervous system lymphoma. Neuro Oncol. 17, 1497–1503 (2015).",
"volume": "17",
"year": "2015"
},
{
"DOI": "10.1016/j.jpsychires.2015.10.003",
"author": "K Ghisoni",
"doi-asserted-by": "publisher",
"first-page": "134",
"journal-title": "J. Psychiatr. Res.",
"key": "8632_CR37",
"unstructured": "Ghisoni, K., de Martins, R. P., Barbeito, L. & Latini, A. Neopterin as a potential cytoprotective brain molecule. J. Psychiatr. Res. 71, 134–139 (2015).",
"volume": "71",
"year": "2015"
},
{
"DOI": "10.1016/j.freeradbiomed.2017.11.022",
"author": "R de Paula Martins",
"doi-asserted-by": "publisher",
"first-page": "371",
"journal-title": "Free Radic. Biol. Med.",
"key": "8632_CR38",
"unstructured": "de Paula Martins, R. et al. Neopterin preconditioning prevents inflammasome activation in mammalian astrocytes. Free Radic. Biol. Med. 115, 371–382 (2018).",
"volume": "115",
"year": "2018"
},
{
"DOI": "10.4161/viru.2.2.15480",
"author": "L Vande Walle",
"doi-asserted-by": "publisher",
"first-page": "162",
"journal-title": "Virulence",
"key": "8632_CR39",
"unstructured": "Vande Walle, L., Kanneganti, T.-D. & Lamkanfi, M. HMGB1 release by inflammasomes. Virulence 2, 162–165 (2011).",
"volume": "2",
"year": "2011"
},
{
"DOI": "10.3389/fimmu.2020.00484",
"author": "H Yang",
"doi-asserted-by": "publisher",
"first-page": "484",
"journal-title": "Front. Immunol.",
"key": "8632_CR40",
"unstructured": "Yang, H., Wang, H. & Andersson, U. Targeting inflammation driven by HMGB1. Front. Immunol. 11, 484 (2020).",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1186/s10020-023-00717-3",
"author": "W Ren",
"doi-asserted-by": "publisher",
"first-page": "117",
"journal-title": "Mol. Med.",
"key": "8632_CR41",
"unstructured": "Ren, W., Zhao, L., Sun, Y., Wang, X. & Shi, X. HMGB1 and Toll-like receptors: Potential therapeutic targets in autoimmune diseases. Mol. Med. 29, 117 (2023).",
"volume": "29",
"year": "2023"
},
{
"DOI": "10.3389/fimmu.2018.03022",
"author": "C Savarin",
"doi-asserted-by": "publisher",
"first-page": "3022",
"journal-title": "Front. Immunol.",
"key": "8632_CR42",
"unstructured": "Savarin, C. & Bergmann, C. C. Fine tuning the cytokine storm by IFN and IL-10 following neurotropic coronavirus encephalomyelitis. Front. Immunol. 9, 3022 (2018).",
"volume": "9",
"year": "2018"
},
{
"DOI": "10.1016/j.yexmp.2020.104474",
"author": "E Lavi",
"doi-asserted-by": "publisher",
"first-page": "104474",
"journal-title": "Exp. Mol. Pathol.",
"key": "8632_CR43",
"unstructured": "Lavi, E. & Cong, L. Type I astrocytes and microglia induce a cytokine response in an encephalitic murine coronavirus infection. Exp. Mol. Pathol. 115, 104474 (2020).",
"volume": "115",
"year": "2020"
},
{
"DOI": "10.1084/jem.20061738",
"author": "MA Kleinschek",
"doi-asserted-by": "publisher",
"first-page": "161",
"journal-title": "J. Exp. Med.",
"key": "8632_CR44",
"unstructured": "Kleinschek, M. A. et al. IL-25 regulates Th17 function in autoimmune inflammation. J. Exp. Med. 204, 161–170 (2007).",
"volume": "204",
"year": "2007"
},
{
"DOI": "10.1074/jbc.M109.025940",
"author": "Y Sonobe",
"doi-asserted-by": "publisher",
"first-page": "31834",
"journal-title": "J. Biol. Chem.",
"key": "8632_CR45",
"unstructured": "Sonobe, Y. et al. Interleukin-25 expressed by brain capillary endothelial cells maintains blood-brain barrier function in a protein kinase Cepsilon-dependent manner. J. Biol. Chem. 284, 31834–31842 (2009).",
"volume": "284",
"year": "2009"
},
{
"DOI": "10.1186/1479-5876-10-239",
"author": "L Aloe",
"doi-asserted-by": "publisher",
"first-page": "239",
"journal-title": "J. Transl. Med.",
"key": "8632_CR46",
"unstructured": "Aloe, L., Rocco, M. L., Bianchi, P. & Manni, L. Nerve growth factor: From the early discoveries to the potential clinical use. J. Transl. Med. 10, 239 (2012).",
"volume": "10",
"year": "2012"
},
{
"DOI": "10.1016/j.cytogfr.2004.01.004",
"author": "RWC Wong",
"doi-asserted-by": "publisher",
"first-page": "147",
"journal-title": "Cytokine Growth Fact. Rev.",
"key": "8632_CR47",
"unstructured": "Wong, R. W. C. & Guillaud, L. The role of epidermal growth factor and its receptors in mammalian CNS. Cytokine Growth Fact. Rev. 15, 147–156 (2004).",
"volume": "15",
"year": "2004"
},
{
"DOI": "10.1038/s41392-022-00997-x",
"author": "Y Fan",
"doi-asserted-by": "publisher",
"first-page": "141",
"journal-title": "Signal Transduct. Target Ther.",
"key": "8632_CR48",
"unstructured": "Fan, Y. et al. SARS-CoV-2 Omicron variant: Recent progress and future perspectives. Signal Transduct. Target Ther. 7, 141 (2022).",
"volume": "7",
"year": "2022"
},
{
"DOI": "10.1186/s12883-023-03399-w",
"author": "T Chang",
"doi-asserted-by": "publisher",
"first-page": "351",
"journal-title": "BMC Neurol.",
"key": "8632_CR49",
"unstructured": "Chang, T. et al. Neurological disorders associated with COVID-19 in Sri Lanka. BMC Neurol. 23, 351 (2023).",
"volume": "23",
"year": "2023"
},
{
"DOI": "10.3389/fimmu.2024.1499082",
"author": "S Gong",
"doi-asserted-by": "publisher",
"first-page": "1499082",
"journal-title": "Front. Immunol.",
"key": "8632_CR50",
"unstructured": "Gong, S. et al. Clinical and immunological features in patients with neuroimmune complications of COVID-19 during Omicron wave in China: A case series. Front. Immunol. 15, 1499082 (2024).",
"volume": "15",
"year": "2024"
},
{
"DOI": "10.1111/ene.16096",
"author": "L Lu",
"doi-asserted-by": "publisher",
"first-page": "e16096",
"journal-title": "Eur. J. Neurol.",
"key": "8632_CR51",
"unstructured": "Lu, L. et al. Neurological complications during the omicron COVID-19 wave in China: A cohort study. Eur. J. Neurol. 31, e16096 (2024).",
"volume": "31",
"year": "2024"
},
{
"DOI": "10.1002/jmv.29648",
"author": "S-Y Chen",
"doi-asserted-by": "publisher",
"first-page": "e29648",
"journal-title": "J. Med. Virol.",
"key": "8632_CR52",
"unstructured": "Chen, S.-Y. et al. Prior COVID-19 vaccination and reduced risk of cerebrovascular diseases among COVID-19 survivors. J. Med. Virol. 96, e29648 (2024).",
"volume": "96",
"year": "2024"
},
{
"DOI": "10.2196/47272",
"author": "M Liu",
"doi-asserted-by": "publisher",
"first-page": "e47272",
"journal-title": "JMIR Public Health Surveill.",
"key": "8632_CR53",
"unstructured": "Liu, M. et al. Immune-boosting effect of the COVID-19 vaccine: Real-world bidirectional cohort study. JMIR Public Health Surveill. 9, e47272 (2023).",
"volume": "9",
"year": "2023"
},
{
"DOI": "10.1016/j.bbi.2023.03.022",
"author": "F Ceban",
"doi-asserted-by": "publisher",
"first-page": "211",
"journal-title": "Brain Behav. Immun.",
"key": "8632_CR54",
"unstructured": "Ceban, F. et al. COVID-19 vaccination for the prevention and treatment of long COVID: A systematic review and meta-analysis. Brain Behav. Immun. 111, 211–229 (2023).",
"volume": "111",
"year": "2023"
},
{
"DOI": "10.1016/S2666-5247(23)00171-4",
"author": "X Zhu",
"doi-asserted-by": "publisher",
"first-page": "e692",
"journal-title": "Lancet Microbe",
"key": "8632_CR55",
"unstructured": "Zhu, X. et al. Dynamics of inflammatory responses after SARS-CoV-2 infection by vaccination status in the USA: A prospective cohort study. Lancet Microbe 4, e692–e703 (2023).",
"volume": "4",
"year": "2023"
},
{
"DOI": "10.1038/s41591-020-0968-3",
"author": "A Gupta",
"doi-asserted-by": "publisher",
"first-page": "1017",
"journal-title": "Nat. Med.",
"key": "8632_CR56",
"unstructured": "Gupta, A. et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 26, 1017–1032 (2020).",
"volume": "26",
"year": "2020"
}
],
"reference-count": 56,
"references-count": 56,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.nature.com/articles/s41598-025-08632-9"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Central nervous system and systemic inflammatory networks associated with acute neurological outcomes in COVID-19",
"type": "journal-article",
"update-policy": "https://doi.org/10.1007/springer_crossmark_policy",
"volume": "15"
}