The influence of temperature, humidity, and simulated sunlight on the infectivity of SARS-CoV-2 in aerosols
et al., Aerosol Science and Technology, doi:10.1080/02786826.2020.1829536, Nov 2020
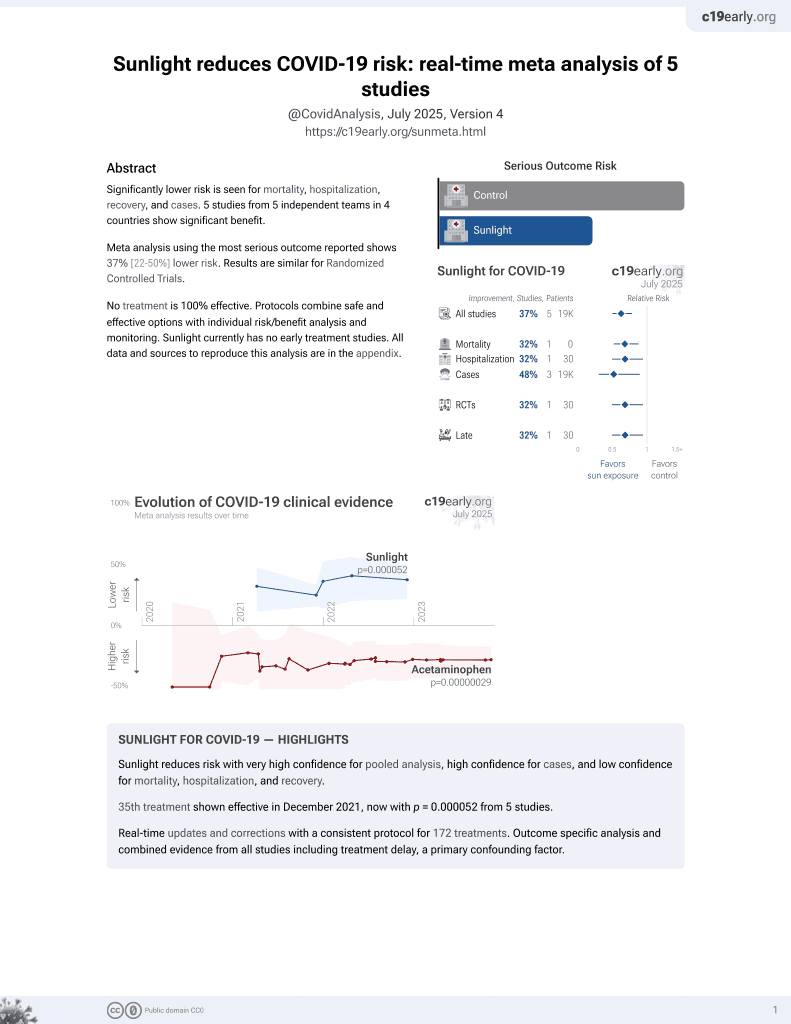
Sunlight for COVID-19
36th treatment shown to reduce risk in
December 2021, now with p = 0.000052 from 5 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
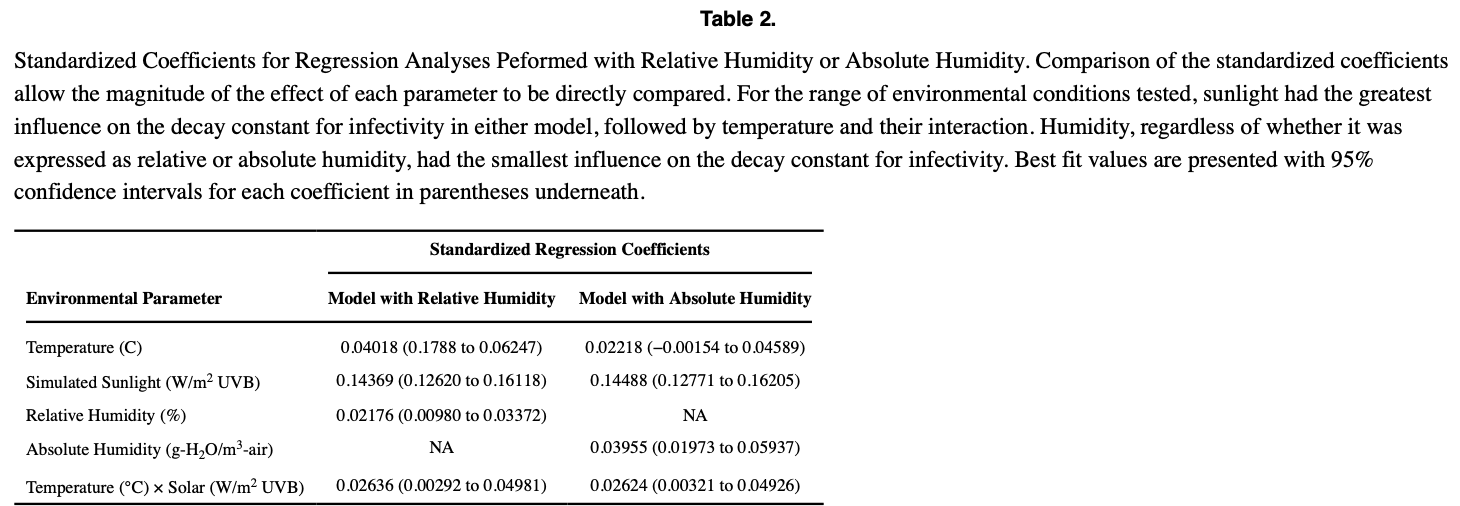
Analysis of the effects of temperature, humidity, and simulated sunlight on the decay rate and infectivity of aerosolized SARS-CoV-2 virus particles. The results showed that higher temperature, lower humidity, and higher simulated sunlight (UVB radiation) exposure resulted in faster decay rates and loss of viral infectivity over time. Across the conditions tested, simulated sunlight had the greatest effect, with infectious virus decreasing by 90% in as little as 4.8 minutes under intense summer sunlight conditions. This suggests that environmental factors like sunlight and temperature may play an important role in viral transmission via aerosols.
Dabisch et al., 2 Nov 2020, USA, peer-reviewed, 18 authors.
The influence of temperature, humidity, and simulated sunlight on the infectivity of SARS-CoV-2 in aerosols
Aerosol Science and Technology, doi:10.1080/02786826.2020.1829536
Recent evidence suggests that respiratory aerosols may play a role in the spread of SARS-CoV-2 during the ongoing COVID-19 pandemic. Our laboratory has previously demonstrated that simulated sunlight inactivated SARS-CoV-2 in aerosols and on surfaces. In the present study, we extend these findings to include the persistence of SARS-CoV-2 in aerosols across a range of temperature, humidity, and simulated sunlight levels using an environmentally controlled rotating drum aerosol chamber. The results demonstrate that temperature, simulated sunlight, and humidity are all significant factors influencing the persistence of infectious SARS-CoV-2 in aerosols, but that simulated sunlight and temperature have a greater influence on decay than humidity across the range of conditions tested. The time needed for a 90% decrease in infectious virus ranged from 4.8 min at 40 °C, 20% relative humidity, and high intensity simulated sunlight representative of noon on a clear day on the summer solstice at 4°N latitude, to greater than two hours under conditions representative of those expected indoors or at night. These results suggest that the persistence of infectious SARS-CoV-2 in naturally occurring aerosols may be affected by environmental conditions, and that aerosolized virus could remain infectious for extended periods of time under some environmental conditions. The present study provides a comprehensive dataset on the influence of environmental parameters on the survival of SARS-CoV-2 in aerosols that can be utilized, along with data on viral shedding from infected individuals and the inhalational infectious dose, to inform future modeling and risk assessment efforts.
References
Barreca, Shimshack, Absolute humidity, temperature, and influenza mortality: 30 years of county-level evidence from the United States, Am. J. Epidemiol, doi:10.1093/aje/kws259
Biryukov, Boydston, Dunning, Yeager, Wood et al., Increasing temperature and relative humidity accelerates inactivation of SARS-CoV-2 on surfaces, mSphere, doi:10.1128/mSphere.00441-20
Casanova, Jeon, Rutala, Weber, Sobsey, Effects of air temperature and relative humidity on coronavirus survival on surfaces, Appl. Environ. Microbiol, doi:10.1128/AEM.02291-09
Chan, Peiris, Lam, Poon, Yuen et al., The effects of temperature and relative humidity on the viability of the SARS coronavirus, Adv. Virol, doi:10.1155/2011/734690
Chao, Wan, Morawska, Johnson, Ristovski et al., Characterization of expiration air jets and droplet size distributions immediately at the mouth opening, J. Aerosol Sci, doi:10.1016/j.jaerosci.2008.10.003
Chia, Coleman, Tan, Ong, Gum et al., Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients, Nat. Commun, doi:10.1038/s41467-020-16670-2
Darnell, Subbarao, Feinstone, Taylor Dr, Inactivation of the coronavirus that induces severe acute respiratory syndrome, SARS-CoV, J. Virol. Methods, doi:10.1016/j.jviromet.2004.06.006
Docherty, Harrison, Green, Hardwick, Pius et al., Features of 20 133 UK patients in hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: prospective observational cohort study, BMJ
Dybwad, Skogan, Aerobiological stabilities of different species of gram-negative bacteria, including well-known biothreat simulants, in single-cell particles and cell clusters of different compositions, Appl. Environ. Microbiol, doi:10.1128/AEM.00823-17
Fears, Klimstra, Duprex, Hartman, Weaver et al., Persistence of severe acute respiratory syndrome coronavirus 2 in aerosol suspensions, Emerg. Infect. Dis, doi:10.3201/eid2609.201806
Guo, Wang, Zhang, Li, Li et al., Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, Emerg. Infect. Dis, doi:10.3201/eid2607.200885
Ijaz, Brunner, Sattar, Nair, Cm, Survival characteristics of airborne human coronavirus 229E, J. General Virol, doi:10.1099/0022-1317-66-12-2743
Johnson, Morawska, The mechanism of breath aerosol formation, J. Aerosol Med. Pulmonary Drug Del, doi:10.1089/jamp.2008.0720
Kesavan, Schepers, Bottiger, Edmonds, UV-C decontamination of aerosolized and surface-bound single spores and bioclusters, Aerosol Sci. Tech, doi:10.1080/02786826.2014.889276
Leung, Chu, Shiu, Chan, Mcdevitt et al., Respiratory virus shedding in exhaled breath and efficacy of face masks, Nat. Med, doi:10.1038/s41591-020-0843-2
Lighthart, Shaffer, Increased airborne bacterial survival as a function of particle content and size, Aerosol Sci. Tech, doi:10.1080/02786829708965483
Lindsley, Blachere, Thewlis, Vishnu, Davis et al., Measurements of airborne influenza virus in aerosol particles from human coughs, PloS One, doi:10.1371/journal.pone.0015100
Liu, Ning, Chen, Guo, Liu et al., Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals, Nature, doi:10.1038/s41586020-2271-3
Lovato, De Filippis, Clinical presentation of COVID-19: A systematic review focusing on upper airway symptoms, Ear Nose Throat J, doi:10.1177/0145561320920762
Mcdevitt, Rudnick, First, Spengler, Role of absolute humidity in the inactivation of influenza viruses on stainless steel surfaces at elevated temperatures, Appl. Environ. Microbiol, doi:10.1128/AEM.02674-09
Morawska, Johnson, Ristovski, Hargreaves, Mengersen et al., Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities, J. Aerosol Sci, doi:10.1016/j.jaerosci.2008.11.002
Prata, Rodrigues, Bermejo, Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil, Sci. Total Environ, doi:10.1016/j.scitotenv.2020.138862
Pyankov, Bodnev, Pyankova, Ie, Survival of aerosolized coronavirus in the ambient air, J. Aerosol Sci, doi:10.1016/j.jaerosci.2017.09.009
Rashed, Kodera, Gomez-Tames, Hirata, Influence of absolute humidity, temperature and population density on COVID-19 Spread and Decay Durations: Multi-Prefecture Study in Japan, IJERPH, doi:10.3390/ijerph17155354
Ratnesar-Shumate, Williams, Green, Krause, Holland et al., Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces, J. Infect Dis, doi:10.1093/infdis/jiaa274
Schuit, Gardner, Wood, Bower, Williams et al., The influence of simulated sunlight on the inactivation of influenza virus in aerosols, J. Infect. Dis, doi:10.1093/infdis/jiz582
Schuit, Ratnesar-Shumate, Yolitz, Williams, Weaver et al., Airborne SARS-CoV-2 Is rapidly inactivated by simulated sunlight, J. Infect. Dis, doi:10.1093/infdis/jiaa334
Sehra, Salciccioli, Wiebe, Fundin, Baker, maximum daily temperature, precipitation, ultra-violet light and rates of transmission of SARS-Cov-2 in the United States, Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am, doi:10.1093/cid/ciaa681
Shaman, Goldstein, Lipsitch, Absolute humidity and pandemic versus epidemic influenza, Am. J. Epidemiol, doi:10.1093/aje/kwq347
Smither, Eastaugh, Findlay, Lever, Experimental aerosol survival of SARS-CoV-2 in artificial saliva and tissue culture media at medium and high humidity, Emerg. Microbes Infect, doi:10.1080/22221751.2020.1777906
Van Doremalen, Bushmaker, Morris, Holbrook, Gamble et al., Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1, New Engl. J. Med, doi:10.1056/NEJMc2004973
Yang, Elankumaran, Marr, Concentrations and size distributions of airborne influenza A viruses measured indoors at a health centre, a day-care centre and on aeroplanes, J. R. Soc. Interface, doi:10.1098/rsif.2010.0686
DOI record:
{
"DOI": "10.1080/02786826.2020.1829536",
"ISSN": [
"0278-6826",
"1521-7388"
],
"URL": "http://dx.doi.org/10.1080/02786826.2020.1829536",
"alternative-id": [
"10.1080/02786826.2020.1829536"
],
"assertion": [
{
"label": "Peer Review Statement",
"name": "peerreview_statement",
"order": 1,
"value": "The publishing and review policy for this title is described in its Aims & Scope."
},
{
"URL": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=uast20",
"label": "Aim & Scope",
"name": "aims_and_scope_url",
"order": 2,
"value": "http://www.tandfonline.com/action/journalInformation?show=aimsScope&journalCode=uast20"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Received",
"name": "received",
"order": 0,
"value": "2020-08-05"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Revised",
"name": "revised",
"order": 1,
"value": "2020-09-18"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Accepted",
"name": "accepted",
"order": 2,
"value": "2020-09-19"
},
{
"group": {
"label": "Publication History",
"name": "publication_history"
},
"label": "Published",
"name": "published",
"order": 3,
"value": "2020-11-02"
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-3181-6825",
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"authenticated-orcid": false,
"family": "Dabisch",
"given": "Paul",
"sequence": "first"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Schuit",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Censeo Insight Inc, Seattle, Washington, USA"
}
],
"family": "Herzog",
"given": "Artemas",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Beck",
"given": "Katie",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Wood",
"given": "Stewart",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Krause",
"given": "Melissa",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Miller",
"given": "David",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Weaver",
"given": "Wade",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Freeburger",
"given": "Denise",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Hooper",
"given": "Idris",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Green",
"given": "Brian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Williams",
"given": "Gregory",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Holland",
"given": "Brian",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Bohannon",
"given": "Jordan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Wahl",
"given": "Victoria",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Yolitz",
"given": "Jason",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Hevey",
"given": "Michael",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "National Biodefense Analysis and Countermeasures Center, Operated by BNBI for the U.S. Department of Homeland Security Science and Technology Directorate, Frederick, Maryland, USA;"
}
],
"family": "Ratnesar-Shumate",
"given": "Shanna",
"sequence": "additional"
}
],
"container-title": "Aerosol Science and Technology",
"container-title-short": "Aerosol Science and Technology",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"www.tandfonline.com"
]
},
"created": {
"date-parts": [
[
2020,
10,
5
]
],
"date-time": "2020-10-05T17:06:55Z",
"timestamp": 1601917615000
},
"deposited": {
"date-parts": [
[
2022,
7,
15
]
],
"date-time": "2022-07-15T14:06:17Z",
"timestamp": 1657893977000
},
"indexed": {
"date-parts": [
[
2023,
12,
26
]
],
"date-time": "2023-12-26T17:52:22Z",
"timestamp": 1703613142392
},
"is-referenced-by-count": 120,
"issue": "2",
"issued": {
"date-parts": [
[
2020,
11,
2
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2021,
2,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "https://www.tandfonline.com/doi/pdf/10.1080/02786826.2020.1829536",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "142-153",
"prefix": "10.1080",
"published": {
"date-parts": [
[
2020,
11,
2
]
]
},
"published-online": {
"date-parts": [
[
2020,
11,
2
]
]
},
"published-print": {
"date-parts": [
[
2021,
2,
1
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"DOI": "10.1093/aje/kws259",
"author": "Barreca A. I.",
"doi-asserted-by": "crossref",
"first-page": "S114",
"journal-title": "Am. J. Epidemiol.",
"key": "CIT0001",
"volume": "176",
"year": "2012"
},
{
"DOI": "10.1128/mSphere.00441-20",
"author": "Biryukov J.",
"doi-asserted-by": "crossref",
"first-page": "e00441",
"issue": "4",
"journal-title": "mSphere",
"key": "CIT0002",
"volume": "5",
"year": "2020"
},
{
"DOI": "10.1128/AEM.02291-09",
"doi-asserted-by": "publisher",
"key": "CIT0003"
},
{
"DOI": "10.1155/2011/734690",
"doi-asserted-by": "publisher",
"key": "CIT0004"
},
{
"DOI": "10.1016/j.jaerosci.2008.10.003",
"doi-asserted-by": "publisher",
"key": "CIT0005"
},
{
"DOI": "10.1038/s41467-020-16670-2",
"doi-asserted-by": "publisher",
"key": "CIT0006"
},
{
"DOI": "10.1016/j.jviromet.2004.06.006",
"doi-asserted-by": "publisher",
"key": "CIT0007"
},
{
"DOI": "10.1136/bmj.m1985",
"doi-asserted-by": "publisher",
"key": "CIT0222"
},
{
"DOI": "10.1128/AEM.00823-17",
"author": "Dybwad M.",
"doi-asserted-by": "crossref",
"first-page": "e00823",
"issue": "18",
"journal-title": "Appl. Environ. Microbiol",
"key": "CIT0008",
"volume": "83",
"year": "2017"
},
{
"DOI": "10.3201/eid2609.201806",
"doi-asserted-by": "publisher",
"key": "CIT0009"
},
{
"DOI": "10.3201/eid2607.200885",
"doi-asserted-by": "publisher",
"key": "CIT0010"
},
{
"DOI": "10.1099/0022-1317-66-12-2743",
"doi-asserted-by": "publisher",
"key": "CIT0011"
},
{
"DOI": "10.1089/jamp.2008.0720",
"doi-asserted-by": "publisher",
"key": "CIT0012"
},
{
"DOI": "10.1080/02786826.2014.889276",
"doi-asserted-by": "publisher",
"key": "CIT0013"
},
{
"DOI": "10.1038/s41591-020-0843-2",
"doi-asserted-by": "publisher",
"key": "CIT0014"
},
{
"DOI": "10.1080/02786829708965483",
"author": "Lighthart B.",
"doi-asserted-by": "crossref",
"first-page": "439",
"issue": "3",
"journal-title": "Aerosol Sci. Tech.",
"key": "CIT0015",
"volume": "27",
"year": "1997"
},
{
"DOI": "10.1371/journal.pone.0015100",
"doi-asserted-by": "publisher",
"key": "CIT0016"
},
{
"DOI": "10.1038/s41586-020-2271-3",
"doi-asserted-by": "publisher",
"key": "CIT0017"
},
{
"DOI": "10.1177/0145561320920762",
"doi-asserted-by": "publisher",
"key": "CIT0018"
},
{
"DOI": "10.1128/AEM.02674-09",
"doi-asserted-by": "publisher",
"key": "CIT0019"
},
{
"DOI": "10.1016/j.jaerosci.2008.11.002",
"doi-asserted-by": "publisher",
"key": "CIT0020"
},
{
"key": "CIT0021",
"unstructured": "National Center for Atmospheric Research. 2020. Tropospheric ultraviolet and visible (TUV) radiation model. Accessed on 28 Jun 2020. https://www2.acom.ucar.edu/modeling/tropospheric-ultraviolet-and-visible-tuv-radiation-model."
},
{
"DOI": "10.1016/j.scitotenv.2020.138862",
"doi-asserted-by": "publisher",
"key": "CIT0022"
},
{
"DOI": "10.1016/j.jaerosci.2017.09.009",
"doi-asserted-by": "publisher",
"key": "CIT0023"
},
{
"DOI": "10.3390/ijerph17155354",
"author": "Rashed E. A.",
"doi-asserted-by": "crossref",
"first-page": "5354",
"issue": "15",
"journal-title": "IJERPH",
"key": "CIT0024",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiaa274",
"author": "Ratnesar-Shumate S.",
"doi-asserted-by": "crossref",
"first-page": "214",
"issue": "2",
"journal-title": "J. Infect Dis.",
"key": "CIT0025",
"volume": "222",
"year": "2020"
},
{
"DOI": "10.1093/infdis/jiz582",
"doi-asserted-by": "publisher",
"key": "CIT0026"
},
{
"DOI": "10.1093/infdis/jiaa334",
"doi-asserted-by": "publisher",
"key": "CIT0027"
},
{
"author": "Sehra S. T.",
"journal-title": "Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am.",
"key": "CIT0028",
"year": "2020"
},
{
"DOI": "10.1093/aje/kwq347",
"doi-asserted-by": "publisher",
"key": "CIT0029"
},
{
"DOI": "10.1080/22221751.2020.1777906",
"doi-asserted-by": "publisher",
"key": "CIT0030"
},
{
"DOI": "10.1056/NEJMc2004973",
"doi-asserted-by": "publisher",
"key": "CIT0031"
},
{
"DOI": "10.1098/rsif.2010.0686",
"doi-asserted-by": "publisher",
"key": "CIT0032"
}
],
"reference-count": 33,
"references-count": 33,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.tandfonline.com/doi/full/10.1080/02786826.2020.1829536"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pollution",
"General Materials Science",
"Environmental Chemistry"
],
"subtitle": [],
"title": "The influence of temperature, humidity, and simulated sunlight on the infectivity of SARS-CoV-2 in aerosols",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1080/tandf_crossmark_01",
"volume": "55"
}