Low Levels of Serum and Intracellular Vitamin C in Hospitalized COVID-19 Patients
et al., Nutrients, doi:10.3390/nu15163653, Aug 2023
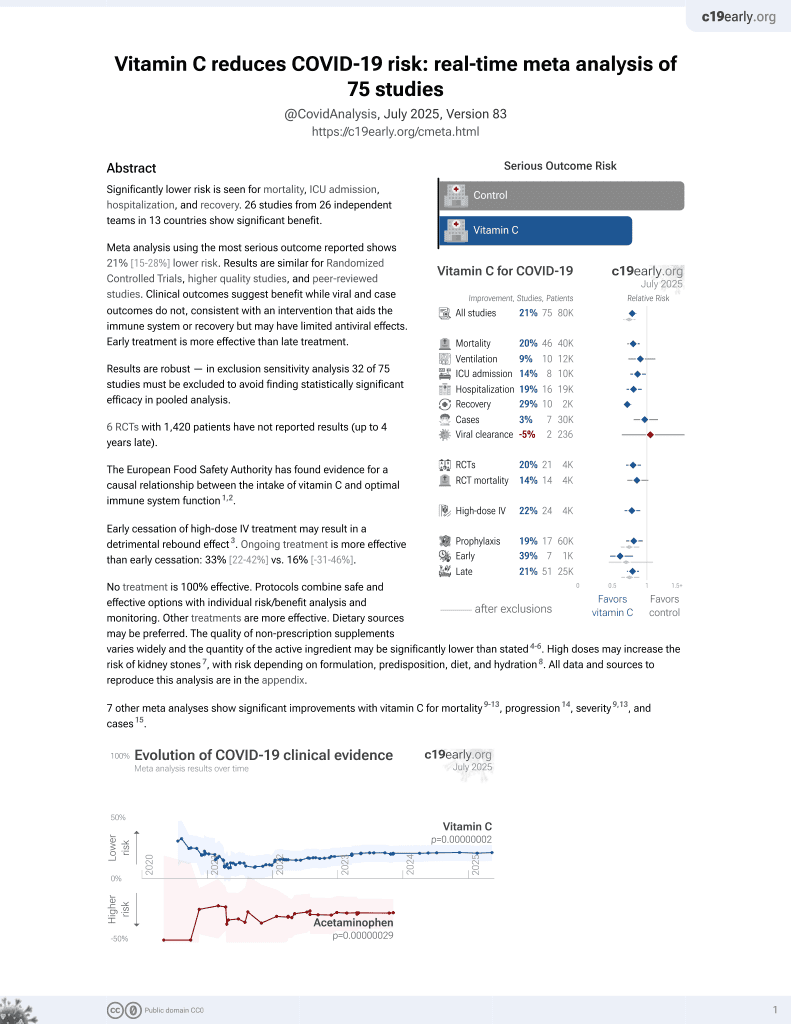
Vitamin C for COVID-19
6th treatment shown to reduce risk in
September 2020, now with p = 0.000000068 from 74 studies, recognized in 22 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
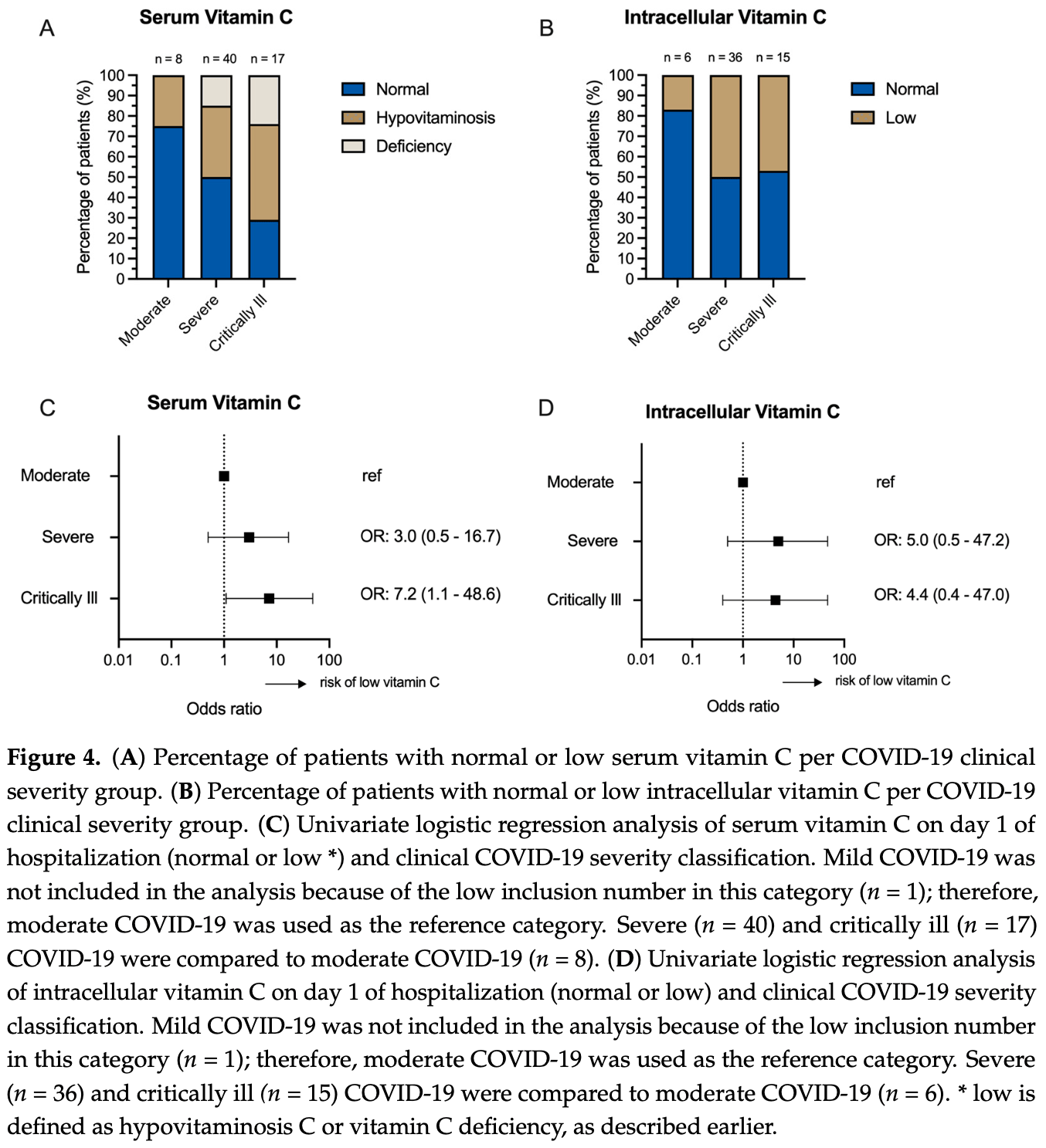
Analysis of serum and intracellular vitamin C levels in hospitalized COVID-19 patients. Low vitamin C levels were common with 36% having serum levels <26 μmol/L and 15% <11 μmol/L.
Intracellular vitamin C levels in peripheral blood mononuclear cells (PBMCs) were low at admission and declined during hospitalization, suggesting ongoing utilization and depletion of vitamin C stores.
Critical patients had higher odds of low serum vitamin C levels. There was a weak negative correlation between serum vitamin C levels and severity, without statistical significance.
|
risk of critical case, 55.9% lower, RR 0.44, p = 0.10, high vitamin C levels (≥26μmol/L) 5 of 34 (14.7%), low vitamin C levels (<26μmol/L) 12 of 36 (33.3%), NNT 5.4.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Boerenkamp et al., 20 Aug 2023, prospective, Netherlands, peer-reviewed, mean age 70.0, 11 authors, study period 2 December, 2020 - 10 March, 2021.
Contact: lara.boerenkamp@mumc.nl (corresponding author).
Low Levels of Serum and Intracellular Vitamin C in Hospitalized COVID-19 Patients
Nutrients, doi:10.3390/nu15163653
Vitamin C is a crucial micronutrient for human immune cell function and has potent antioxidant properties. It is hypothesized that vitamin C serum levels decline during infection. However, the precise mechanisms remain unknown. To gain deeper insights into the true role of vitamin C during infections, we aimed to evaluate the body's vitamin C storage during a SARS-CoV-2 infection. In this single-center study, we examined serum and intracellular vitamin C levels in peripheral blood mononuclear cells (PBMCs) of 70 hospitalized COVID-19 patients on the first and fifth days of hospitalization. Also, clinical COVID-19 severity was evaluated at these timepoints. Our findings revealed a high prevalence of hypovitaminosis C and vitamin C deficiency in hospitalized COVID-19 patients (36% and 15%). Moreover, patients with severe or critical disease exhibited a higher prevalence of low serum vitamin C levels than those with moderate illness. Serum vitamin C levels had a weak negative correlation with clinical COVID-19 severity classification on the day of hospitalization; however, there was no correlation with intracellular vitamin C. Intracellular vitamin C levels were decreased in this cohort as compared to a healthy cohort and showed further decline during hospitalization, while serum levels showed no relevant change. Based on this observation, it can be suggested that the reduction of intracellular vitamin C may be attributed to its antioxidative function, the need for replenishing serum levels, or enhanced turnover by immune cells. These data give an incentive to further investigate the role of intracellular vitamin C in a larger and more heterogeneous cohort as well as the underlying mechanisms.
Conflicts of Interest: The authors declare no conflict of interest.
References
Agarwal, Basmaji, Fernando, Ge, Xiao et al., Parenteral Vitamin C in Patients with Severe Infection: A Systematic Review, doi:10.1056/EVIDoa2200105
Arvinte, Singh, Marik, Serum Levels of Vitamin C and Vitamin D in a Cohort of Critically Ill COVID-19 Patients of a North American Community Hospital Intensive Care Unit in May 2020: A Pilot Study
Bendich, Machlin, Scandurra, Burton, Wayner, The antioxidant role of vitamin C, Adv. Free Radic. Biol. Med, doi:10.1016/S8755-9668(86)80021-7
Bergsten, Amitai, Kehrl, Dhariwal, Klein et al., Millimolar concentrations of ascorbic acid in purified human mononuclear leukocytes. Depletion and reaccumulation, J. Biol. Chem, doi:10.1016/S0021-9258(19)39841-2
Boretti, Banik, Intravenous vitamin C for reduction of cytokines storm in acute respiratory distress syndrome. PharmaNutrition 2020, doi:10.1016/j.phanu.2020.100190
Bozonet, Carr, Pullar, Vissers, Enhanced human neutrophil vitamin C status, chemotaxis and oxidant genera-tion following dietary supplementation with vitamin C-rich SunGold kiwifruit, Nutrients, doi:10.3390/nu7042574
Bozonet, Carr, The Role of Physiological Vitamin C Concentrations on Key Functions of Neutrophils Isolated from Healthy Individuals, Nutrients, doi:10.3390/nu11061363
Canoy, Wareham, Welch, Bingham, Luben et al., Plasma ascorbic acid concentrations and fat distribution in 19 068 British men and women in the European Prospective Investigation into Cancer and Nutrition Norfolk cohort study, Am. J. Clin. Nutr, doi:10.1093/ajcn/82.6.1203
Carr, Bozonet, Pullar, Spencer, Rosengrave et al., Neutrophils Isolated from Septic Patients Exhibit Elevated Uptake of Vitamin C and Normal Intracellular Concentrations despite a Low Vitamin C Milieu, Antioxidants
Carr, Maggini, Vitamin C and Immune Function, Nutrients, doi:10.3390/nu9111211
Carr, Rosengrave, Bayer, Chambers, Mehrtens et al., Hypovitaminosis C and vitamin C deficiency in criti-cally ill patients despite recommended enteral and parenteral intakes, Crit. Care, doi:10.1186/s13054-017-1891-y
Fain, Pariés, Jacquart Bt Le Moël, Kettaneh, Stirnemann et al., Hypovitaminosis C in hospitalized patients, Eur. J. Intern. Med, doi:10.1016/j.ejim.2003.08.006
Galan, Viteri, Bertrais, Czernichow, Faure et al., Serum concentrations of β-carotene, vitamins C and E, zinc and selenium are influenced by sex, age, diet, smoking status, alcohol consumption and corpulence in a general French adult population, Eur. J. Clin. Nutr, doi:10.1038/sj.ejcn.1602230
Hasselholt, Tveden-Nyborg, Lykkesfeldt, Distribution of vitamin C is tissue specific with early saturation of the brain and adrenal glands following differential oral dose regimens in guinea pigs, Br. J. Nutr, doi:10.1017/S0007114515000690
Hemilä, Chalker, Vitamin C for preventing and treating the common cold, Cochrane Database Syst. Rev, doi:10.1002/14651858.CD000980.pub4
Hemilä, Vitamin C and Infections, Nutrients, doi:10.3390/nu9040339
Hong, Kim, Kang, Lee, Hwang, Vitamin C is taken up by human T cells via sodium-dependent vitamin C transporter 2 (SVCT 2 ) and exerts inhibitory effects on the activation of these cells in vitro, Anat. Cell Biol, doi:10.5115/acb.2016.49.2.88
Huijskens, Walczak, Koller, Briedé, Senden-Gijsbers et al., Technical Advance: Ascorbic acid induces development of double-positive T cells from human hematopoietic stem cells in the absence of stromal cells, J. Leukoc. Biol, doi:10.1189/jlb.1TA0214-121RR
Huijskens, Walczak, Sarkar, Atrafi, Senden-Gijsbers et al., Ascorbic acid promotes proliferation of natural killer cell populations in culture systems applicable for natural killer cell therapy, Cytotherapy, doi:10.1016/j.jcyt.2015.01.004
Hyder Pottoo, Abu-Izneid, Mohammad Ibrahim, Noushad Javed, Alhajri et al., Immune system re-sponse during viral Infections: Immunomodulators, cytokine storm (CS) and Immunotherapeutics in COVID-19. Saudi, Pharm. J. 2021, doi:10.1016/j.jsps.2020.12.018
Levine, Conry-Cantilena, Wang, Welch, Washko et al., Vitamin C pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance, Proc. Natl. Acad. Sci, doi:10.1073/pnas.93.8.3704
Manning, Mitchell, Appadurai, Shakya, Pierce et al., None, Vitamin C Promotes Maturation of T-Cells. Antioxid. Redox Signal, doi:10.1089/ars.2012.4988
Mccall, Clark, Luben, Wareham, Khaw et al., Plasma Vitamin C Levels: Risk Factors for Deficiency and Association with Self-Reported Functional Health in the European Prospective Investigation into Cancer-Norfolk, Nutrients, doi:10.3390/nu11071552
Mehta, Mcauley, Brown, Sanchez, Tattersall et al., UK. COVID-19: Consider cytokine storm syndromes and immunosuppression, Lancet, doi:10.1016/S0140-6736(20)30628-0
Metnitz, Bartens, Fischer, Fridrich, Steltzer et al., Antioxidant status in patients with acute respiratory dis-tress syndrome, Intensive Care Med, doi:10.1007/s001340050813
Mueller, Rouse, Immune responses to viruses, Clin. Immunol, doi:10.1016/B978-0-323-04404-2.10027-2
Nabzdyk, Bittner, Vitamin C in the critically ill-Indications and controversies, World J. Crit. Care Med, doi:10.5492/wjccm.v7.i5.52
Nhcotpsro, Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment, 7th Edition, shtml
Omaye, Schaus, Kutnink, Hawkes, Measurement of vitamin C in blood components by high-performance liq-uid chromatography. Implication in assessing vitamin C status, Ann. N. Y. Acad Sci, doi:10.1111/j.1749-6632.1987.tb23776.x
Padayatty, Levine, Vitamin C: The known and the unknown and Goldilocks, Oral Dis, doi:10.1111/odi.12446
Patterson, Isales, Fulzele, Low level of Vitamin C and dysregulation of Vitamin C transporter might be involved in the severity of COVID-19 Infection, Aging Dis, doi:10.14336/AD.2020.0918
Praveen, Puvvada, Association of vitamin C status in diabetes mellitus: Prevalence and predictors of vitamin C defi-ciency, Future J. Pharm. Sci
Putzu, Daems, Lopez-Delgado, Giordano, Landoni, The Effect of Vitamin C on Clinical Outcome in Critically Ill Patients: A Systematic Review With Meta-Analysis of Randomized Controlled Trials, Crit. Care Med, doi:10.1097/CCM.0000000000003700
Ran, Zhao, Wang, Wang, Zhao et al., Extra Dose of Vitamin C Based on a Daily Supplementation Shortens the Common Cold: A Meta-Analysis of 9 Randomized Controlled Trials, BioMed Res. Int, doi:10.1155/2018/1837634
Rawat, Roy, Maitra, Gulati, Khanna et al., Vitamin C and COVID-19 treatment: A systematic review and me-ta-analysis of randomized controlled trials, Diabetes Metab. Syndr. Clin. Res. Rev. 2021, doi:10.1016/j.dsx.2021.102324
Rowe, Carr, Global Vitamin C Status and Prevalence of Deficiency: A Cause for Concern?, Nutrients, doi:10.3390/nu12072008
Savini, Rossi, Pierro, Avigliano, Catani, SVCT1 and SVCT2: Key proteins for vitamin C uptake, Amino Acids, doi:10.1007/s00726-007-0555-7
Schleicher, Carroll, Ford, Lacher, Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003-2004 National Health and Nutrition Examination Survey (NHANES), Am. J. Clin. Nutr, doi:10.3945/ajcn.2008.27016
Schlueter, Johnston, Vitamin C: Overview and update, J. Evid. Based Complement. Altern. Med
Schorah, Downing, Piripitsi, Gallivan, Al-Hazaa et al., Total vitamin C, ascorbic acid, and dehy-droascorbic acid concentrations in plasma of critically ill patients, Am. J. Clin. Nutr, doi:10.1093/ajcn/63.5.760
Ströhle, Wolters, Hahn, Micronutrients at the interface between inflammation and infection ascorbic acid and calciferol. Part 1: General overview with a focus on ascorbic acid, Inflamm. Allergy-Drug Targets, doi:10.2174/187152811794352105
Tomasa-Irriguible, Bielsa-Berrocal, COVID-19: Up to 82% critically ill patients had low Vitamin C values, Nutr. J, doi:10.1186/s12937-021-00727-z
Van Gorkom, Gijsbers, Ververs, El Molla, Sarodnik et al., Easy-to-Use HPLC Method to Measure Intra-cellular Ascorbic Acid Levels in Human Peripheral Blood Mononuclear Cells and in Plasma, Antioxidants, doi:10.3390/antiox11010134
Van Gorkom, Klein Wolterink, Van Elssen, Wieten, Germeraad et al., Influence of Vitamin C on Lymphocytes: An Overview, Antioxidants, doi:10.3390/antiox7030041
Wang, Yang, Pei, Chong, Guo et al., SAA, LDH, and DD predict poor prognosis of coronavirus disease (COVID-19): A meta-analysis from 7739 patients, Scand. J. Clin. Lab. Investig
Yang, Hu, Huang, Xiong, Sun, The prognostic value of the SOFA score in patients with COVID-19: A retrospective, observational study, Medicine, doi:10.1097/MD.0000000000026900
Zabet, Mohammadi, Ramezani, Khalili, Effect of high-dose Ascorbic acid on vasopressor s requirement in septic shock, J. Res. Pharm. Pract
Zhang, Jativa, Vitamin C supplementation in the critically ill: A systematic review and meta-analysis, SAGE Open Med, doi:10.1177/2050312118807615
DOI record:
{
"DOI": "10.3390/nu15163653",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu15163653",
"abstract": "<jats:p>Vitamin C is a crucial micronutrient for human immune cell function and has potent antioxidant properties. It is hypothesized that vitamin C serum levels decline during infection. However, the precise mechanisms remain unknown. To gain deeper insights into the true role of vitamin C during infections, we aimed to evaluate the body’s vitamin C storage during a SARS-CoV-2 infection. In this single-center study, we examined serum and intracellular vitamin C levels in peripheral blood mononuclear cells (PBMCs) of 70 hospitalized COVID-19 patients on the first and fifth days of hospitalization. Also, clinical COVID-19 severity was evaluated at these timepoints. Our findings revealed a high prevalence of hypovitaminosis C and vitamin C deficiency in hospitalized COVID-19 patients (36% and 15%). Moreover, patients with severe or critical disease exhibited a higher prevalence of low serum vitamin C levels than those with moderate illness. Serum vitamin C levels had a weak negative correlation with clinical COVID-19 severity classification on the day of hospitalization; however, there was no correlation with intracellular vitamin C. Intracellular vitamin C levels were decreased in this cohort as compared to a healthy cohort and showed further decline during hospitalization, while serum levels showed no relevant change. Based on this observation, it can be suggested that the reduction of intracellular vitamin C may be attributed to its antioxidative function, the need for replenishing serum levels, or enhanced turnover by immune cells. These data give an incentive to further investigate the role of intracellular vitamin C in a larger and more heterogeneous cohort as well as the underlying mechanisms.</jats:p>",
"alternative-id": [
"nu15163653"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-6870-1992",
"affiliation": [
{
"name": "Division of Hematology, Department of Internal Medicine, GROW School for Oncology and Developmental Biology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"authenticated-orcid": false,
"family": "Boerenkamp",
"given": "Lara S.",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Division of Hematology, Department of Internal Medicine, GROW School for Oncology and Developmental Biology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"family": "Gijsbers",
"given": "Birgit L. M. G.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Hematology, Department of Internal Medicine, GROW School for Oncology and Developmental Biology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"family": "Ververs",
"given": "Erik-Jan",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Internal Medicine, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"family": "Pijpers",
"given": "Eva M. S.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-3062-2612",
"affiliation": [
{
"name": "Department of Internal Medicine, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"authenticated-orcid": false,
"family": "Spaetgens",
"given": "Bart",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Hematology, Department of Internal Medicine, GROW School for Oncology and Developmental Biology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"family": "de Coninck",
"given": "Aniek",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Hematology, Department of Internal Medicine, GROW School for Oncology and Developmental Biology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"family": "Germeraad",
"given": "Wilfred T. V.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Central Diagnostic Laboratory, Department of Clinical Chemistry, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"family": "Wodzig",
"given": "Will K. W. H.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Department of Transplantation Immunology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"family": "Wieten",
"given": "Lotte",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7327-7834",
"affiliation": [
{
"name": "Division of Hematology, Department of Internal Medicine, GROW School for Oncology and Developmental Biology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"authenticated-orcid": false,
"family": "van Gorkom",
"given": "Gwendolyn N. Y.",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-1784-1765",
"affiliation": [
{
"name": "Division of Hematology, Department of Internal Medicine, GROW School for Oncology and Developmental Biology, Maastricht University Medical Center, 6229 HX Maastricht, The Netherlands"
}
],
"authenticated-orcid": false,
"family": "van Elssen",
"given": "Catharina H. M. J.",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2023,
8,
21
]
],
"date-time": "2023-08-21T05:46:56Z",
"timestamp": 1692596816000
},
"deposited": {
"date-parts": [
[
2023,
8,
21
]
],
"date-time": "2023-08-21T06:54:54Z",
"timestamp": 1692600894000
},
"indexed": {
"date-parts": [
[
2023,
8,
22
]
],
"date-time": "2023-08-22T05:04:06Z",
"timestamp": 1692680646109
},
"is-referenced-by-count": 0,
"issue": "16",
"issued": {
"date-parts": [
[
2023,
8,
20
]
]
},
"journal-issue": {
"issue": "16",
"published-online": {
"date-parts": [
[
2023,
8
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
8,
20
]
],
"date-time": "2023-08-20T00:00:00Z",
"timestamp": 1692489600000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/15/16/3653/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "3653",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2023,
8,
20
]
]
},
"published-online": {
"date-parts": [
[
2023,
8,
20
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1016/S8755-9668(86)80021-7",
"article-title": "The antioxidant role of vitamin C",
"author": "Bendich",
"doi-asserted-by": "crossref",
"first-page": "419",
"journal-title": "Adv. Free Radic. Biol. Med.",
"key": "ref_1",
"volume": "2",
"year": "1986"
},
{
"DOI": "10.5492/wjccm.v7.i5.52",
"article-title": "Vitamin C in the critically ill—Indications and controversies",
"author": "Nabzdyk",
"doi-asserted-by": "crossref",
"first-page": "52",
"journal-title": "World J. Crit. Care Med.",
"key": "ref_2",
"volume": "7",
"year": "2018"
},
{
"DOI": "10.1177/1533210110392951",
"article-title": "Vitamin C: Overview and update",
"author": "Schlueter",
"doi-asserted-by": "crossref",
"first-page": "49",
"journal-title": "J. Evid. Based Complement. Altern. Med.",
"key": "ref_3",
"volume": "16",
"year": "2011"
},
{
"DOI": "10.1016/j.phanu.2020.100190",
"article-title": "Intravenous vitamin C for reduction of cytokines storm in acute respiratory distress syndrome",
"author": "Boretti",
"doi-asserted-by": "crossref",
"first-page": "100190",
"journal-title": "PharmaNutrition",
"key": "ref_4",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3390/nu11061363",
"doi-asserted-by": "crossref",
"key": "ref_5",
"unstructured": "Bozonet, S.M., and Carr, A.C. (2019). The Role of Physiological Vitamin C Concentrations on Key Functions of Neutrophils Isolated from Healthy Individuals. Nutrients, 11."
},
{
"DOI": "10.3390/nu7042574",
"article-title": "Enhanced human neutrophil vitamin C status, chemotaxis and oxidant genera-tion following dietary supplementation with vitamin C-rich SunGold kiwifruit",
"author": "Bozonet",
"doi-asserted-by": "crossref",
"first-page": "2574",
"journal-title": "Nutrients",
"key": "ref_6",
"volume": "7",
"year": "2015"
},
{
"DOI": "10.1111/odi.12446",
"article-title": "Vitamin C: The known and the unknown and Goldilocks",
"author": "Padayatty",
"doi-asserted-by": "crossref",
"first-page": "463",
"journal-title": "Oral Dis.",
"key": "ref_7",
"volume": "22",
"year": "2016"
},
{
"DOI": "10.1189/jlb.1TA0214-121RR",
"article-title": "Technical Advance: Ascorbic acid induces development of double-positive T cells from human hematopoietic stem cells in the absence of stromal cells",
"author": "Huijskens",
"doi-asserted-by": "crossref",
"first-page": "1165",
"journal-title": "J. Leukoc. Biol.",
"key": "ref_8",
"volume": "96",
"year": "2014"
},
{
"DOI": "10.1089/ars.2012.4988",
"article-title": "Vitamin C Promotes Maturation of T-Cells",
"author": "Manning",
"doi-asserted-by": "crossref",
"first-page": "2054",
"journal-title": "Antioxid. Redox Signal",
"key": "ref_9",
"volume": "19",
"year": "2013"
},
{
"DOI": "10.3390/nu9111211",
"doi-asserted-by": "crossref",
"key": "ref_10",
"unstructured": "Carr, A.C., and Maggini, S. (2017). Vitamin C and Immune Function. Nutrients, 9."
},
{
"DOI": "10.1016/j.jcyt.2015.01.004",
"article-title": "Ascorbic acid promotes proliferation of natural killer cell populations in culture systems applicable for natural killer cell therapy",
"author": "Huijskens",
"doi-asserted-by": "crossref",
"first-page": "613",
"journal-title": "Cytotherapy",
"key": "ref_11",
"volume": "17",
"year": "2015"
},
{
"DOI": "10.1111/j.1749-6632.1987.tb23776.x",
"article-title": "Measurement of vitamin C in blood components by high-performance liq-uid chromatography. Implication in assessing vitamin C status",
"author": "Omaye",
"doi-asserted-by": "crossref",
"first-page": "389",
"journal-title": "Ann. N. Y. Acad Sci.",
"key": "ref_12",
"volume": "498",
"year": "1987"
},
{
"DOI": "10.3390/antiox7030041",
"doi-asserted-by": "crossref",
"key": "ref_13",
"unstructured": "Van Gorkom, G.N.Y., Klein Wolterink, R.G.J., Van Elssen, C.H.M.J., Wieten, L., Germeraad, W.T.V., and Bos, G.M.J. (2018). Influence of Vitamin C on Lymphocytes: An Overview. Antioxidants, 7."
},
{
"DOI": "10.5115/acb.2016.49.2.88",
"article-title": "Vitamin C is taken up by human T cells via sodium-dependent vitamin C transporter 2 (SVCT2) and exerts inhibitory effects on the activation of these cells in vitro",
"author": "Hong",
"doi-asserted-by": "crossref",
"first-page": "88",
"journal-title": "Anat. Cell Biol.",
"key": "ref_14",
"volume": "49",
"year": "2016"
},
{
"DOI": "10.1016/S0021-9258(19)39841-2",
"article-title": "Millimolar concentrations of ascorbic acid in purified human mononuclear leukocytes. Depletion and reaccumulation",
"author": "Bergsten",
"doi-asserted-by": "crossref",
"first-page": "2584",
"journal-title": "J. Biol. Chem.",
"key": "ref_15",
"volume": "265",
"year": "1990"
},
{
"DOI": "10.1007/s00726-007-0555-7",
"article-title": "SVCT1 and SVCT2: Key proteins for vitamin C uptake",
"author": "Savini",
"doi-asserted-by": "crossref",
"first-page": "347",
"journal-title": "Amino Acids",
"key": "ref_16",
"volume": "34",
"year": "2007"
},
{
"DOI": "10.1017/S0007114515000690",
"article-title": "Distribution of vitamin C is tissue specific with early saturation of the brain and adrenal glands following differential oral dose regimens in guinea pigs",
"author": "Hasselholt",
"doi-asserted-by": "crossref",
"first-page": "1539",
"journal-title": "Br. J. Nutr.",
"key": "ref_17",
"volume": "113",
"year": "2015"
},
{
"DOI": "10.1073/pnas.93.8.3704",
"article-title": "Vitamin C pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance",
"author": "Levine",
"doi-asserted-by": "crossref",
"first-page": "3704",
"journal-title": "Proc. Natl. Acad. Sci. USA",
"key": "ref_18",
"volume": "93",
"year": "1996"
},
{
"DOI": "10.1093/ajcn/82.6.1203",
"article-title": "Plasma ascorbic acid concentrations and fat distribution in 19 068 British men and women in the European Prospective Investigation into Cancer and Nutrition Norfolk cohort study",
"author": "Canoy",
"doi-asserted-by": "crossref",
"first-page": "1203",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_19",
"volume": "82",
"year": "2005"
},
{
"DOI": "10.3390/nu12072008",
"doi-asserted-by": "crossref",
"key": "ref_20",
"unstructured": "Rowe, S., and Carr, A.C. (2020). Global Vitamin C Status and Prevalence of Deficiency: A Cause for Concern?. Nutrients, 12."
},
{
"DOI": "10.1016/j.ejim.2003.08.006",
"article-title": "Hypovitaminosis C in hospitalized patients",
"author": "Fain",
"doi-asserted-by": "crossref",
"first-page": "419",
"journal-title": "Eur. J. Intern. Med.",
"key": "ref_21",
"volume": "14",
"year": "2003"
},
{
"DOI": "10.3390/nu9040339",
"doi-asserted-by": "crossref",
"key": "ref_22",
"unstructured": "Hemilä, H. (2017). Vitamin C and Infections. Nutrients, 9."
},
{
"DOI": "10.1186/s13054-017-1891-y",
"article-title": "Hypovitaminosis C and vitamin C deficiency in criti-cally ill patients despite recommended enteral and parenteral intakes",
"author": "Carr",
"doi-asserted-by": "crossref",
"first-page": "300",
"journal-title": "Crit. Care",
"key": "ref_23",
"volume": "21",
"year": "2017"
},
{
"DOI": "10.1007/s001340050813",
"article-title": "Antioxidant status in patients with acute respiratory dis-tress syndrome",
"author": "Metnitz",
"doi-asserted-by": "crossref",
"first-page": "180",
"journal-title": "Intensive Care Med.",
"key": "ref_24",
"volume": "25",
"year": "1999"
},
{
"DOI": "10.1093/ajcn/63.5.760",
"article-title": "Total vitamin C, ascorbic acid, and dehy-droascorbic acid concentrations in plasma of critically ill patients",
"author": "Schorah",
"doi-asserted-by": "crossref",
"first-page": "760",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_25",
"volume": "63",
"year": "1996"
},
{
"DOI": "10.1080/00365513.2021.2000635",
"article-title": "CRP, SAA, LDH, and DD predict poor prognosis of coronavirus disease (COVID-19): A meta-analysis from 7739 patients",
"author": "Wang",
"doi-asserted-by": "crossref",
"first-page": "679",
"journal-title": "Scand. J. Clin. Lab. Investig.",
"key": "ref_26",
"volume": "81",
"year": "2021"
},
{
"DOI": "10.1097/CCM.0000000000003700",
"article-title": "The Effect of Vitamin C on Clinical Outcome in Critically Ill Patients: A Systematic Review With Meta-Analysis of Randomized Controlled Trials",
"author": "Putzu",
"doi-asserted-by": "crossref",
"first-page": "774",
"journal-title": "Crit. Care Med.",
"key": "ref_27",
"volume": "47",
"year": "2019"
},
{
"DOI": "10.1177/2050312118807615",
"article-title": "Vitamin C supplementation in the critically ill: A systematic review and meta-analysis",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "2050312118807615",
"journal-title": "SAGE Open Med.",
"key": "ref_28",
"volume": "6",
"year": "2018"
},
{
"DOI": "10.4103/2279-042X.179569",
"article-title": "Effect of high-dose Ascorbic acid on vasopressor′s requirement in septic shock",
"author": "Zabet",
"doi-asserted-by": "crossref",
"first-page": "94",
"journal-title": "J. Res. Pharm. Pract.",
"key": "ref_29",
"volume": "5",
"year": "2016"
},
{
"article-title": "Vitamin C for preventing and treating the common cold",
"author": "Chalker",
"first-page": "CD000980",
"journal-title": "Cochrane Database Syst. Rev.",
"key": "ref_30",
"volume": "2013",
"year": "2013"
},
{
"DOI": "10.1016/S0140-6736(20)30628-0",
"article-title": "COVID-19: Consider cytokine storm syndromes and immunosuppression",
"author": "Mehta",
"doi-asserted-by": "crossref",
"first-page": "1033",
"journal-title": "Lancet",
"key": "ref_31",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.2174/187152811794352105",
"article-title": "Micronutrients at the interface between inflammation and infection ascorbic acid and calciferol. Part 1: General overview with a focus on ascorbic acid",
"author": "Wolters",
"doi-asserted-by": "crossref",
"first-page": "54",
"journal-title": "Inflamm. Allergy-Drug Targets",
"key": "ref_32",
"volume": "10",
"year": "2011"
},
{
"DOI": "10.3390/antiox10101607",
"doi-asserted-by": "crossref",
"key": "ref_33",
"unstructured": "Carr, A.C., Bozonet, S., Pullar, J., Spencer, E., Rosengrave, P., and Shaw, G. (2021). Neutrophils Isolated from Septic Patients Exhibit Elevated Uptake of Vitamin C and Normal Intracellular Concentrations despite a Low Vitamin C Milieu. Antioxidants, 10."
},
{
"key": "ref_34",
"unstructured": "NHCotPsRo (2021, November 01). Chinese Clinical Guidance for COVID-19 Pneumonia Diagnosis and Treatment, 7th Edition 2020. China, Available online: http://www.nhc.gov.cn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989.shtml."
},
{
"DOI": "10.1097/MD.0000000000026900",
"article-title": "The prognostic value of the SOFA score in patients with COVID-19: A retrospective, observational study",
"author": "Yang",
"doi-asserted-by": "crossref",
"first-page": "e26900",
"journal-title": "Medicine",
"key": "ref_35",
"volume": "100",
"year": "2021"
},
{
"DOI": "10.3390/antiox11010134",
"doi-asserted-by": "crossref",
"key": "ref_36",
"unstructured": "van Gorkom, G., Gijsbers, B., Ververs, E.-J., El Molla, A., Sarodnik, C., Riess, C., Wodzig, W., Bos, G., and Van Elssen, C. (2022). Easy-to-Use HPLC Method to Measure Intra-cellular Ascorbic Acid Levels in Human Peripheral Blood Mononuclear Cells and in Plasma. Antioxidants, 11."
},
{
"DOI": "10.1159/000434757",
"doi-asserted-by": "crossref",
"key": "ref_37",
"unstructured": "German Nutrition Society (2015). New Reference Values for Vitamin C Intake. Ann. Nutr. Metab., 67, 13–20."
},
{
"DOI": "10.1016/j.medidd.2020.100064",
"article-title": "Serum Levels of Vitamin C and Vitamin D in a Cohort of Critically Ill COVID-19 Patients of a North American Community Hospital Intensive Care Unit in May 2020: A Pilot Study",
"author": "Arvinte",
"doi-asserted-by": "crossref",
"first-page": "100064",
"journal-title": "Med. Drug Discov.",
"key": "ref_38",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.14336/AD.2020.0918",
"article-title": "Low level of Vitamin C and dysregulation of Vitamin C transporter might be involved in the severity of COVID-19 Infection",
"author": "Patterson",
"doi-asserted-by": "crossref",
"first-page": "14",
"journal-title": "Aging Dis.",
"key": "ref_39",
"volume": "12",
"year": "2021"
},
{
"DOI": "10.1186/s12937-021-00727-z",
"article-title": "COVID-19: Up to 82% critically ill patients had low Vitamin C values",
"doi-asserted-by": "crossref",
"first-page": "66",
"journal-title": "Nutr. J.",
"key": "ref_40",
"volume": "20",
"year": "2021"
},
{
"DOI": "10.1038/sj.ejcn.1602230",
"article-title": "Serum concentrations of β-carotene, vitamins C and E, zinc and selenium are influenced by sex, age, diet, smoking status, alcohol consumption and corpulence in a general French adult population",
"author": "Galan",
"doi-asserted-by": "crossref",
"first-page": "1181",
"journal-title": "Eur. J. Clin. Nutr.",
"key": "ref_41",
"volume": "59",
"year": "2005"
},
{
"DOI": "10.3390/nu11071552",
"doi-asserted-by": "crossref",
"key": "ref_42",
"unstructured": "McCall, S.J., Clark, A.B., Luben, R.N., Wareham, N.J., Khaw, K.-T., and Myint, P.K. (2019). Plasma Vitamin C Levels: Risk Factors for Deficiency and Association with Self-Reported Functional Health in the European Prospective Investigation into Cancer-Norfolk. Nutrients, 11."
},
{
"DOI": "10.1016/j.jsps.2020.12.018",
"article-title": "Immune system re-sponse during viral Infections: Immunomodulators, cytokine storm (CS) and Immunotherapeutics in COVID-19",
"author": "AlHajri",
"doi-asserted-by": "crossref",
"first-page": "173",
"journal-title": "Saudi. Pharm. J.",
"key": "ref_43",
"volume": "29",
"year": "2021"
},
{
"DOI": "10.1016/B978-0-323-04404-2.10027-2",
"doi-asserted-by": "crossref",
"key": "ref_44",
"unstructured": "Mueller, S.N., and Rouse, B.T. (2008). Immune responses to viruses. Clin. Immunol., 421–431."
},
{
"DOI": "10.1186/s43094-020-00040-2",
"article-title": "Association of vitamin C status in diabetes mellitus: Prevalence and predictors of vitamin C defi-ciency",
"author": "Praveen",
"doi-asserted-by": "crossref",
"first-page": "30",
"journal-title": "Future J. Pharm. Sci.",
"key": "ref_45",
"volume": "6",
"year": "2020"
},
{
"DOI": "10.3945/ajcn.2008.27016",
"article-title": "Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES)",
"author": "Schleicher",
"doi-asserted-by": "crossref",
"first-page": "1252",
"journal-title": "Am. J. Clin. Nutr.",
"key": "ref_46",
"volume": "90",
"year": "2009"
},
{
"DOI": "10.1056/EVIDoa2200105",
"article-title": "Parenteral Vitamin C in Patients with Severe Infection: A Systematic Review",
"author": "Agarwal",
"doi-asserted-by": "crossref",
"first-page": "e33989",
"journal-title": "NEJM Evid.",
"key": "ref_47",
"volume": "1",
"year": "2022"
},
{
"DOI": "10.1016/j.dsx.2021.102324",
"article-title": "Vitamin C and COVID-19 treatment: A systematic review and me-ta-analysis of randomized controlled trials",
"author": "Rawat",
"doi-asserted-by": "crossref",
"first-page": "102324",
"journal-title": "Diabetes Metab. Syndr. Clin. Res. Rev.",
"key": "ref_48",
"volume": "15",
"year": "2021"
},
{
"DOI": "10.1155/2018/1837634",
"article-title": "Extra Dose of Vitamin C Based on a Daily Supplementation Shortens the Common Cold: A Meta-Analysis of 9 Randomized Controlled Trials",
"author": "Ran",
"doi-asserted-by": "crossref",
"first-page": "1837634",
"journal-title": "BioMed Res. Int.",
"key": "ref_49",
"volume": "2018",
"year": "2018"
}
],
"reference-count": 49,
"references-count": 49,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/15/16/3653"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Low Levels of Serum and Intracellular Vitamin C in Hospitalized COVID-19 Patients",
"type": "journal-article",
"volume": "15"
}