Nutritional Risk Assessment Scores Effectively Predict Mortality in Critically Ill Patients with Severe COVID-19
et al., Nutrients, doi:10.3390/nu14102105, May 2022
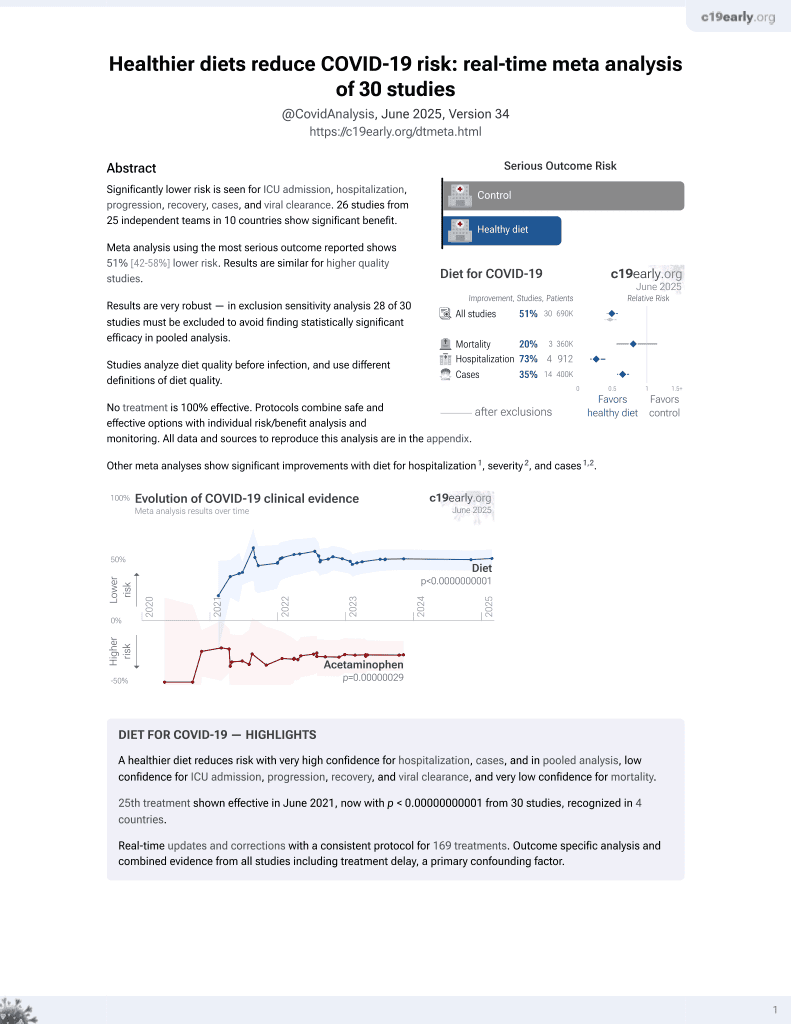
Diet for COVID-19
26th treatment shown to reduce risk in
June 2021, now with p < 0.00000000001 from 30 studies, recognized in 4 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 90 severe COVID-19 ARDS patients in Romania, showing nutritional risk assessment scores PNI, CONUT, NUTRIC, and mNUTRIC to be independent predictors of mortality.
Bodolea et al., 18 May 2022, retrospective, Romania, peer-reviewed, survey, median age 67.0, 8 authors, study period December 2020 - March 2021.
Contact: avram.lucretia9@gmail.com (corresponding author), cbodolea@gmail.com, andrada.nemes@ymail.com, mihaela_cocis@yahoo.com, eu_cristina_oana@yahoo.fr, crisan.dc@gmail.com, mihaela_c87@yahoo.com, craciun.rares.calin@elearn.umfcluj.ro.
Nutritional Risk Assessment Scores Effectively Predict Mortality in Critically Ill Patients with Severe COVID-19
Nutrients, doi:10.3390/nu14102105
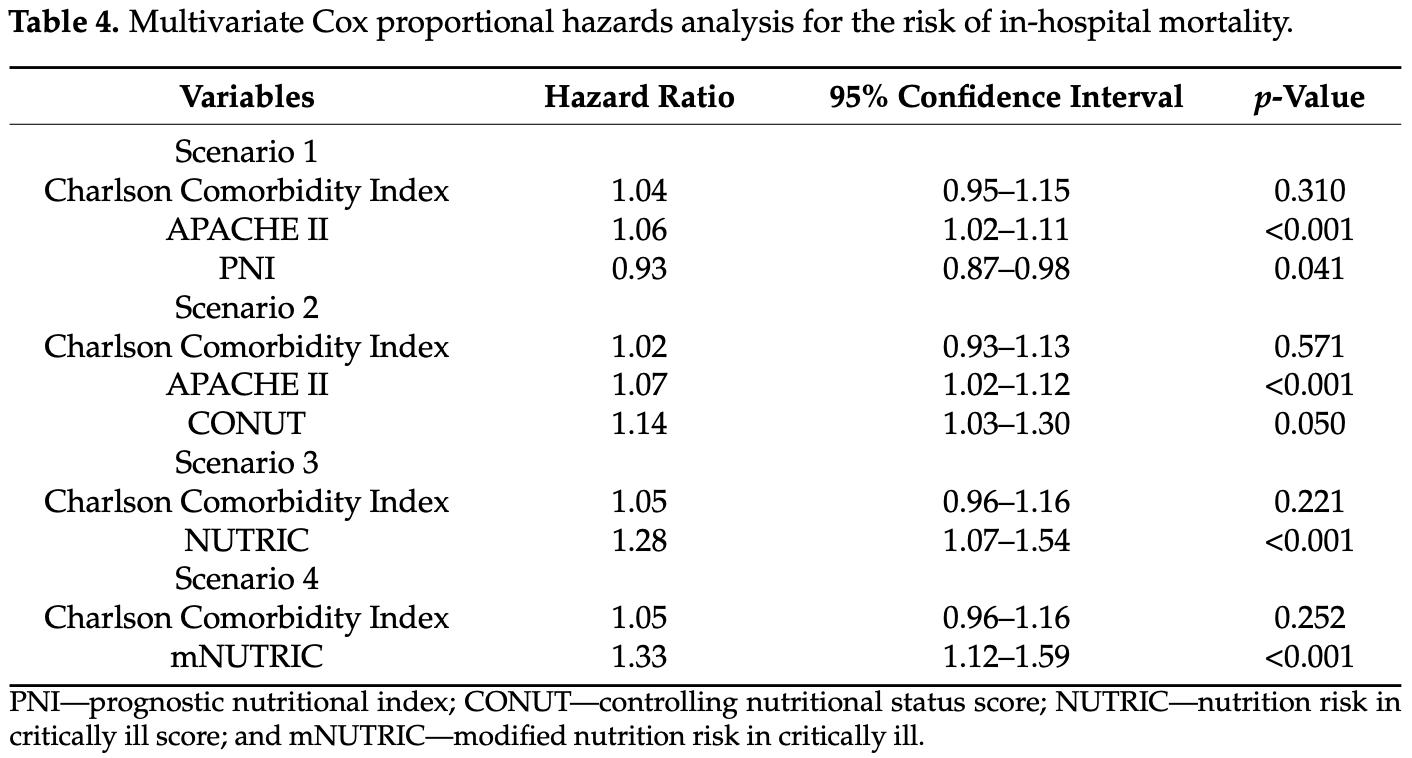
Background: Malnutrition predicts a worse outcome for critically ill patients. However, quick, easy-to-use nutritional risk assessment tools have not been adequately validated. Aims and Methods: The study aimed to evaluate the role of four biological nutritional risk assessment instruments (the Prognostic Nutritional Index-PNI, the Controlling Nutritional Status Score-CONUT, the Nutrition Risk in Critically Ill-NUTRIC, and the modified NUTRIC-mNUTRIC), along with CT-derived fat tissue and muscle mass measurements in predicting in-hospital mortality in a consecutive series of 90 patients hospitalized in the intensive care unit for COVID-19-associated ARDS. Results: In-hospital mortality was 46.7% (n = 42/90). Non-survivors had a significantly higher nutritional risk, as expressed by all four scores. All scores were independent predictors of mortality on the multivariate regression models. PNI had the best discriminative capabilities for mortality, with an area under the curve (AUC) of 0.77 for a cut-off value of 28.05. All scores had an AUC above 0.72. The volume of fat tissue and muscle mass were not associated with increased mortality risk. Conclusions: PNI, CONUT, NUTRIC, and mNUTRIC are valuable nutritional risk assessment tools that can accurately predict mortality in critically ill patients with COVID-19-associated ARDS.
Conflicts of Interest: The authors declare no conflict of interest.
References
Abate, Chekole, Estifanos, Abate, Kabthymer, Prevalence and Outcomes of Malnutrition among Hospitalized COVID-19 Patients: A Systematic Review and Meta-Analysis, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.03.002
Bengelloun, Ortega, Ancochea, Sanz-Garcia, Rodríguez-Serrano et al., Usefulness of the CONUT Index upon Hospital Admission as a Potential Prognostic Indicator of COVID-19 Health Outcomes, Chin. Med. J, doi:10.1097/CM9.0000000000001798
Besutti, Pellegrini, Ottone, Cantini, Milic et al., The Impact of Chest CT Body Composition Parameters on Clinical Outcomes in COVID-19 Patients, PLoS ONE, doi:10.1371/journal.pone.0251768
Booth, Reed, Ponzo, Yassaee, Aral et al., Population Risk Factors for Severe Disease and Mortality in COVID-19: A Global Systematic Review and Meta-Analysis, PLoS ONE, doi:10.1371/journal.pone.0247461
Calder, Nutrition and Immunity: Lessons for COVID-19, Nutr. Diabetes, doi:10.1038/s41387-021-00165-0
Cederholm, Jensen, Correia, Gonzalez, Fukushima et al., GLIM Criteria for the Diagnosis of Malnutrition-A Consensus Report from the Global Clinical Nutrition Community, J. Cachexia Sarcopenia Muscle, doi:10.1002/jcsm.12383
Charlson, Pompei, Ales, Mackenzie, A New Method of Classifying Prognostic in Longitudinal Studies: Development and Validation, J. Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Cheng, Sung, Cheng, Hsu, Guo et al., Prognostic Nutritional Index and the Risk of Mortality in Patients With Acute Heart Failure, J. Am. Heart Assoc, doi:10.1161/JAHA.116.004876
De Ulíbarri, González-Madroño, De Vilar, González, González et al., CONUT: A Tool for Controlling Nutritional Status. First Validation in a Hospital Population, Nutr. Hosp
Heyland, Dhaliwal, Jiang, Day, Identifying Critically Ill Patients Who Benefit the Most from Nutrition Therapy: The Development and Initial Validation of a Novel Risk Assessment Tool, Crit. Care, doi:10.1186/cc10546
Hu, Deng, Wang, Chen, Gu et al., Predictive Value of the Prognostic Nutritional Index for the Severity of Coronavirus Disease, Nutrition, doi:10.1016/j.nut.2020.111123
Hu, Guo, Zhou, Shi, Characteristics of SARS-CoV-2 and COVID-19, Nat. Rev. Microbiol
Knaus, Draper, Wagner, Zimmerman, APACHE II: A Severity of Disease Classification System, Crit. Care Med, doi:10.1097/00003246-198510000-00009
Kosovali, Kucuk, Soyal, Mutlu, Can Prognostic Nutritional Index Predict Mortality in Intensive Care Patients with COVID-19?, Int. J. Clin. Pract, doi:10.1111/ijcp.14800
Kumar, Kumar, Kumar, Pattanayak, Singh et al., Nutric Score as a Predictor of Outcome in COVID-19 ARDS Patients: A Retrospective Observational Study, Indian J. Anaesth, doi:10.4103/ija.ija_474_21
Kurtz, Grant, Marano, Arrieta, Grant et al., Long-Term Effects of Malnutrition on Severity of COVID-19, Sci. Rep, doi:10.1038/s41598-021-94138-z
Li, Fang, Li, Pan, Qin et al., CT Image Visual Quantitative Evaluation and Clinical Classification of Coronavirus Disease (COVID-19), Eur. Radiol, doi:10.1007/s00330-020-06817-6
Li, Zhou, Ba, Wang, Song et al., Nutritional Risk and Therapy for Severe and Critical COVID-19 Patients: A Multicenter Retrospective Observational Study, Clin. Nutr
Liberti, Piacentino, Umbrello, Muttini, Comparison between Nutric Score and Modified Nutric Score to Assess ICU Mortality in Critically Ill Patients with COVID-19, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2021.04.026
Loi, Wang, Ong, Lee, Nutritional Support of Critically Ill Adults and Children with Acute Respiratory Distress Syndrome: A Clinical Review, Clin. Nutr. ESPEN, doi:10.1016/j.clnesp.2017.02.005
Lu, Ren, Jiang, The Relationship between Prognostic Nutritional Index and All-Cause Mortality in Critically Ill Patients: A Retrospective Study, Int. J. Gen. Med, doi:10.2147/IJGM.S318896
Moctezuma-Velazquez, Miranda-Zazueta, Ortiz-Brizuela, Gonzalez-Lara, Tamez-Torres et al., Low Thoracic Skeletal Muscle Area Is Not Associated with Negative Outcomes in Patients with COVID-19, Am. J. Phys. Med. Rehabil, doi:10.1097/PHM.0000000000001716
Mueller, Compher, Ellen, American Society for Parenteral and Enteral Nutrition (ASPEN) Board of Directors. Clinical Guidelines-Nutrition Screening, Assessment, and Intervention in Adults, J. Parenter. Enter. Nutr, doi:10.1177/0148607110389335
Onodera, Goseki, Kosaki, Prognostic Nutritional Index in Gastrointestinal Surgery of Malnourished Cancer Patients] Japanese, Nihon Geka Gekkai Zasshi
Poros, Becker-Pennrich, Sabel, Stemmler, Wassilowsky et al., Anthropometric Analysis of Body Habitus and Outcomes in Critically Ill COVID-19 Patients, Obes. Med, doi:10.1016/j.obmed.2021.100358
Rahman, Hasan, Agarwala, Martin, Day et al., Identifying Critically-Ill Patients Who Will Benefit Most from Nutritional Therapy: Further Validation of the "Modified NUTRIC" Nutritional Risk Assessment Tool, Clin. Nutr, doi:10.1016/j.clnu.2015.01.015
Schiaffino, Albano, Cozzi, Messina, Arioli et al., CT-Derived Chest Muscle Metrics for Outcome Prediction in Patients with COVID-19, Radiology, doi:10.1148/radiol.2021204141
Shao, Lai, Duan, Ge, Ye, Nutritional Indices at Admission Are Associated with Mortality Rates of Patients in the Intensive Care Unit, Eur. J. Clin. Nutr, doi:10.1038/s41430-021-00994-3
Shimoyama, Umegaki, Kadono, Minami, Presepsin Values and Prognostic Nutritional Index Predict Mortality in Intensive Care Unit Patients with Sepsis: A Pilot Study, BMC Res. Notes, doi:10.1186/s13104-021-05659-9
Shirakabe, Hata, Kobayashi, Okazaki, Matsushita et al., The Prognostic Impact of Malnutrition in Patients with Severely Decompensated Acute Heart Failure, as Assessed Using the Prognostic Nutritional Index (PNI) and Controlling Nutritional Status (CONUT) Score, Heart Vessel, doi:10.1007/s00380-017-1034-z
Singer, Blaser, Berger, Alhazzani, Calder et al., ESPEN Guideline on Clinical Nutrition in the Intensive Care Unit, Clin. Nutr, doi:10.1016/j.clnu.2018.08.037
Song, Ma, Wang, Qin, Xu et al., Nutritional Screening Based on Objective Indices at Admission Predicts In-Hospital Mortality in Patients with COVID-19, Nutr. J, doi:10.1186/s12937-021-00702-8
Sugita, Miyazaki, Shimada, Shimizu, Kunimoto et al., Correlation of Nutritional Indices on Admission to the Coronary Intensive Care Unit with the Development of Delirium, Nutrients, doi:10.3390/nu10111712
Sun, Chen, Xu, Li, He, The Prognostic Significance of the Prognostic Nutritional Index in Cancer: A Systematic Review and Meta-Analysis, J. Cancer Res. Clin. Oncol, doi:10.1007/s00432-014-1714-3
Taylor, Marson, Elhadi, Macleod, Yu et al., Factors Associated with Mortality in Patients with COVID-19 Admitted to Intensive Care: A Systematic Review and Meta-Analysis, Anaesthesia, doi:10.1111/anae.15532
Thibault, Seguin, Tamion, Pichard, Singer, Nutrition of the COVID-19 Patient in the Intensive Care Unit (ICU): A Practical Guidance, Crit. Care, doi:10.1186/s13054-020-03159-z
Tseng, Tu, Chen, Wang, Chen et al., Significance of the Modified Nutric Score for Predicting Clinical Outcomes in Patients with Severe Community-Acquired Pneumonia, Nutrients, doi:10.3390/nu14010198
Van Heusden, Swartz, Chargi, De Jong, Van Baal et al., Feasibility of Assessment of Skeletal Muscle Mass on a Single Cross-Sectional Image at the Level of the Fourth Thoracic Vertebra, Eur. J. Radiol, doi:10.1016/j.ejrad.2021.109879
Vincent, Moreno, Takala, Willatts, De Mendonça et al., The SOFA (Sepsis-Related Organ Failure Assessment) Score to Describe Organ Dysfunction/Failure, Intensive Care Med
Wang, He, Kang, Jianguo, Controlling Nutritional Status (CONUT) Score Is a Predictive Marker for Patients with Traumatic Brain Injury, Clin. Neurol. Neurosurg, doi:10.1016/j.clineuro.2020.105909
Wang, Lin, Wei, Li, Liao et al., Predictive Value of Prognostic Nutritional Index on COVID-19 Severity, Front. Nutr, doi:10.3389/fnut.2020.582736
Wei, Wu, Jin, Mu, Gu et al., Predictive Significance of the Prognostic Nutritional Index (PNI) in Patients with Severe COVID-19, J. Immunol. Res, doi:10.1155/2021/9917302
Zhang, He, Yu, Peng, Feng et al., The Modified NUTRIC Score Can Be Used for Nutritional Risk Assessment as Well as Prognosis Prediction in Critically Ill COVID-19 Patients, Clin. Nutr
Zhou, Ma, Xiang, Tao, Yu et al., A Correlation Analysis Between the Nutritional Status and Prognosis of COVID-19 Patients, J. Nutr. Health Aging, doi:10.1007/s12603-020-1457-6
DOI record:
{
"DOI": "10.3390/nu14102105",
"ISSN": [
"2072-6643"
],
"URL": "http://dx.doi.org/10.3390/nu14102105",
"abstract": "<jats:p>Background: Malnutrition predicts a worse outcome for critically ill patients. However, quick, easy-to-use nutritional risk assessment tools have not been adequately validated. Aims and Methods: The study aimed to evaluate the role of four biological nutritional risk assessment instruments (the Prognostic Nutritional Index—PNI, the Controlling Nutritional Status Score—CONUT, the Nutrition Risk in Critically Ill—NUTRIC, and the modified NUTRIC—mNUTRIC), along with CT-derived fat tissue and muscle mass measurements in predicting in-hospital mortality in a consecutive series of 90 patients hospitalized in the intensive care unit for COVID-19-associated ARDS. Results: In-hospital mortality was 46.7% (n = 42/90). Non-survivors had a significantly higher nutritional risk, as expressed by all four scores. All scores were independent predictors of mortality on the multivariate regression models. PNI had the best discriminative capabilities for mortality, with an area under the curve (AUC) of 0.77 for a cut-off value of 28.05. All scores had an AUC above 0.72. The volume of fat tissue and muscle mass were not associated with increased mortality risk. Conclusions: PNI, CONUT, NUTRIC, and mNUTRIC are valuable nutritional risk assessment tools that can accurately predict mortality in critically ill patients with COVID-19-associated ARDS.</jats:p>",
"alternative-id": [
"nu14102105"
],
"author": [
{
"ORCID": "http://orcid.org/0000-0001-7798-0762",
"affiliation": [],
"authenticated-orcid": false,
"family": "Bodolea",
"given": "Constantin",
"sequence": "first"
},
{
"affiliation": [],
"family": "Nemes",
"given": "Andrada",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0003-2656-3234",
"affiliation": [],
"authenticated-orcid": false,
"family": "Avram",
"given": "Lucretia",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-5872-8630",
"affiliation": [],
"authenticated-orcid": false,
"family": "Craciun",
"given": "Rares",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Coman",
"given": "Mihaela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ene-Cocis",
"given": "Mihaela",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ciobanu",
"given": "Cristina",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Crisan",
"given": "Dana",
"sequence": "additional"
}
],
"container-title": "Nutrients",
"container-title-short": "Nutrients",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
5,
19
]
],
"date-time": "2022-05-19T03:14:26Z",
"timestamp": 1652930066000
},
"deposited": {
"date-parts": [
[
2022,
5,
19
]
],
"date-time": "2022-05-19T03:32:50Z",
"timestamp": 1652931170000
},
"indexed": {
"date-parts": [
[
2022,
5,
19
]
],
"date-time": "2022-05-19T04:12:59Z",
"timestamp": 1652933579800
},
"is-referenced-by-count": 0,
"issue": "10",
"issued": {
"date-parts": [
[
2022,
5,
18
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2022,
5
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
5,
18
]
],
"date-time": "2022-05-18T00:00:00Z",
"timestamp": 1652832000000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2072-6643/14/10/2105/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "2105",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2022,
5,
18
]
]
},
"published-online": {
"date-parts": [
[
2022,
5,
18
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1038/s41579-020-00459-7",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1111/anae.15532",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1371/journal.pone.0247461",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1038/s41387-021-00165-0",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.clnesp.2021.03.002",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"DOI": "10.1038/s41598-021-94138-z",
"doi-asserted-by": "publisher",
"key": "ref6"
},
{
"DOI": "10.1016/j.clnu.2018.08.037",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1186/s13054-020-03159-z",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"DOI": "10.1016/j.clnesp.2017.02.005",
"doi-asserted-by": "publisher",
"key": "ref9"
},
{
"DOI": "10.1177/0148607110389335",
"doi-asserted-by": "publisher",
"key": "ref10"
},
{
"article-title": "[Prognostic Nutritional Index in Gastrointestinal Surgery of Malnourished Cancer Patients] Japanese",
"author": "Onodera",
"first-page": "1001",
"journal-title": "Nihon Geka Gekkai Zasshi",
"key": "ref11",
"volume": "85",
"year": "1984"
},
{
"article-title": "CONUT: A Tool for Controlling Nutritional Status. First Validation in a Hospital Population",
"author": "Ignacio de Ulíbarri",
"first-page": "38",
"journal-title": "Nutr. Hosp.",
"key": "ref12",
"volume": "20",
"year": "2005"
},
{
"DOI": "10.1186/cc10546",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/j.clnu.2015.01.015",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1016/j.ejrad.2021.109879",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1148/radiol.2021204141",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.1097/PHM.0000000000001716",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1097/00003246-198510000-00009",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.1007/BF01709751",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1007/s00330-020-06817-6",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1371/journal.pone.0251768",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"DOI": "10.1007/s00432-014-1714-3",
"doi-asserted-by": "publisher",
"key": "ref23"
},
{
"DOI": "10.1161/JAHA.116.004876",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.2147/IJGM.S318896",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.3389/fnut.2020.582736",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/j.nut.2020.111123",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1155/2021/9917302",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1186/s13104-021-05659-9",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1111/ijcp.14800",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.3390/nu10111712",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"DOI": "10.1016/j.clineuro.2020.105909",
"doi-asserted-by": "publisher",
"key": "ref32"
},
{
"DOI": "10.1007/s00380-017-1034-z",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1038/s41430-021-00994-3",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1097/CM9.0000000000001798",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1186/s12937-021-00702-8",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1007/s12603-020-1457-6",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1016/j.clnu.2020.09.040",
"doi-asserted-by": "publisher",
"key": "ref38"
},
{
"DOI": "10.1016/j.clnesp.2021.04.026",
"doi-asserted-by": "publisher",
"key": "ref39"
},
{
"DOI": "10.1016/j.clnu.2020.05.051",
"doi-asserted-by": "publisher",
"key": "ref40"
},
{
"DOI": "10.4103/ija.ija_474_21",
"doi-asserted-by": "publisher",
"key": "ref41"
},
{
"DOI": "10.3390/nu14010198",
"doi-asserted-by": "publisher",
"key": "ref42"
},
{
"DOI": "10.1002/jcsm.12383",
"doi-asserted-by": "publisher",
"key": "ref43"
},
{
"DOI": "10.1016/j.obmed.2021.100358",
"doi-asserted-by": "publisher",
"key": "ref44"
}
],
"reference-count": 44,
"references-count": 44,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2072-6643/14/10/2105"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Food Science",
"Nutrition and Dietetics"
],
"subtitle": [],
"title": "Nutritional Risk Assessment Scores Effectively Predict Mortality in Critically Ill Patients with Severe COVID-19",
"type": "journal-article",
"volume": "14"
}