Clinical Predictors of Mortality and Critical Illness in Patients with COVID-19 Pneumonia
et al., Metabolites, doi:10.3390/metabo11100679, Oct 2021
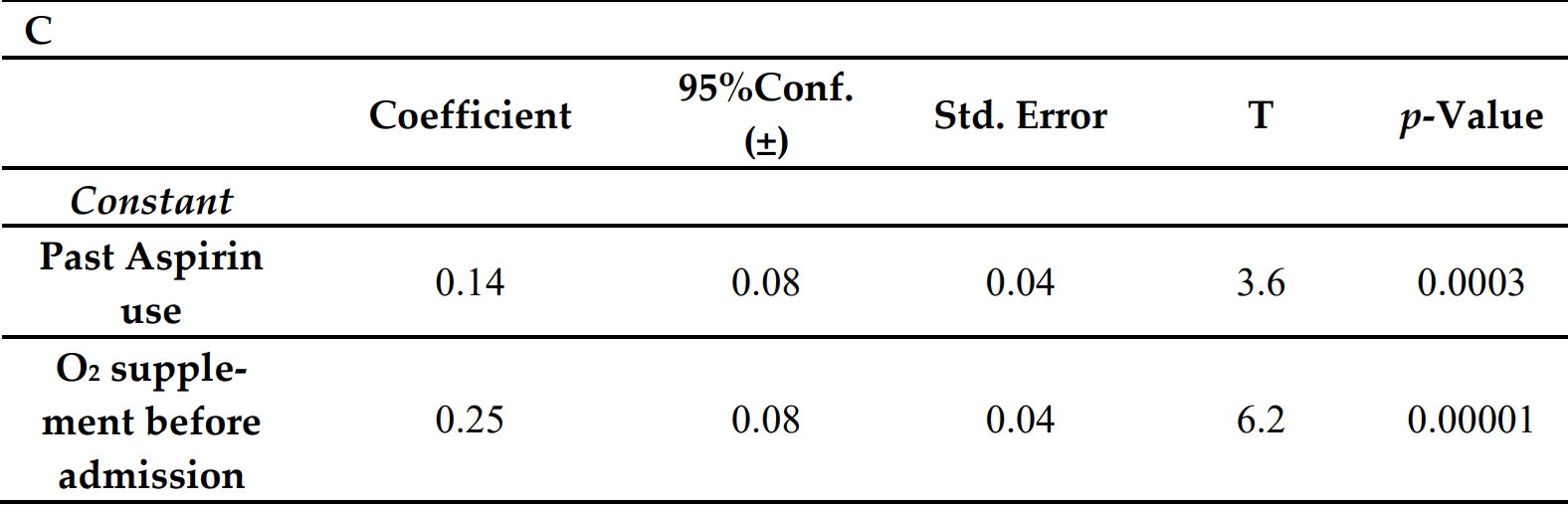
Retrospective 390 hospitalized patients in Israel, showing higher risk of mortality with prior aspirin use. Details of the analysis are not provided.
|
risk of death, 13.0% higher, RR 1.13, p < 0.001, treatment 45 of 140 (32.1%), control 29 of 250 (11.6%), adjusted per study, odds ratio converted to relative risk, group sizes approximated (only percentages provided).
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Basheer et al., 2 Oct 2021, retrospective, Israel, peer-reviewed, 4 authors.
Clinical Predictors of Mortality and Critical Illness in Patients with COVID-19 Pneumonia
Metabolites, doi:10.3390/metabo11100679
Background/Aim: Early identification of patients with COVID-19 who will develop severe or critical disease symptoms is important for delivering proper and early treatment. We analyzed demographic, clinical, immunological, hematological, biochemical and radiographic findings that may be of utility to clinicians in predicting COVID-19 severity and mortality. Methods: Electronic medical record data from patients diagnosed with COVID-19 from November 2020 to June 2021 in the COVID-19 Department in the Galilee Medical Center, Nahariya, Israel, were collected. Epidemiologic, clinical, laboratory and imaging variables were analyzed. Multivariate stepwise regression analyses and discriminant analyses were used to identify and validate powerful predictors. The main outcome measure was invasive ventilation, or death. Results: The study population included 390 patients, with a mean age of 61 ± 18, and 51% were male. The non-survivors were mostly male, elderly and overweight and significantly suffered from hypertension, diabetes mellitus type 2, lung disease, hemodialysis and past use of aspirin. Four predictive factors were found that associated with increased disease severity and/or mortality: age, NLR, BUN, and use of high flow oxygen therapy (HFNC). The AUC or diagnostic accuracy was 87%, with a sensitivity of 97%, specificity of 60%, PPV of 87% and NPP of 91%. The cytokine levels of CXCL-10, GCSF, IL-2 and IL-6 were significantly reduced upon the discharge of severely ill COVID-19 patients. Conclusions: The predictive factors associated with increased mortality include age, NLR, BUN, and use of HFNC upon admission. Identifying those with higher risks of mortality could help in early interventions to reduce the risk of death.
Conflicts of Interest: The authors declare no conflict of interest.
Abbreviations BUN: Blood urea nitrogen; NLR: Neutrophil to lymphocyte ratio; HFNC: High flow nasal cannula
References
Aziz, Haghbin, Lee-Smith, Goyal, Nawras et al., Gastrointestinal predictors of severe COVID-19: Systematic review and meta-analysis, Ann. Gastroenterol
Boyle, Di Gangi, Hamid, Mottram, Mcnamee et al., Aspirin therapy in patients with acute respiratory distress syndrome (ARDS) is associated with reduced intensive care unit mortality: A prospective analysis, Crit. Care
Brisco, Zile, Ter Maaten, Hanberg, Wilson et al., The risk of death associated with proteinuria in heart failure is restricted to patients with an elevated blood urea nitrogen to creatinine ratio, Int. J. Cardiol
Caricchio, Gallucci, Dass, Zhang, Gallucci et al., Temple University COVID-19 Research Group. Preliminary predictive criteria for COVID-19 cytokine storm, Ann. Rheum. Dis
Chen, Janz, Bastarache, May, O'neal et al., Prehospital aspirin use is associated with reduced risk of acute respiratory distress syndrome in critically ill patients: A propensity-adjusted analysis, Crit. Care Med
Chen, Zhao, Qu, Chen, Xiong et al., Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely associated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients, Clin Infect Dis
Cheng, Luo, Wang, Zhang, Wang et al., Kidney disease is associated with inhospital death of patients with COVID-19, Kidney Int
Chinnadurai, Ogedengbe, Agarwal, Money-Coomes, Abdurrahman et al., Older age and frailty are the chief predictors of mortality in COVID-19 patients admitted to an acute medical unit in a secondary care setting-a cohort study, BMC Geriatr
Chu, Kim, Young, Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): A systematic review and meta-analysis, Lancet
Di Angelantonio, Bhupathiraju, Wormser, Gao, Kaptoge et al., Body-mass index and all-cause mortality: Individual-participant-data meta-analysis of 239 prospective studies in four continents, Lancet
Duan, Liu, Li, Zhang, Yu et al., Effectiveness of convalescent plasma therapy in severe COVID-19 patients
Erlich, Talmor, Cartin-Ceba, Gajic, Kor, Prehospitalization antiplatelet therapy is associated with a reduced incidence of acute lung injury: A population-based cohort study, Chest
Gotsman, Zwas, Planer, Admon, Lotan et al., The significance of serum urea and renal function in patients with heart failure, Medicine
Hendren, Drazner, Bozkurt, Cooper, Jr, Description and proposed management of the acute COVID-19 cardiovascular syndrome, Circulation
Iqbal, Lam, Sounderajah, Clarke, Ashrafian et al., Characteristics and predictors of acute and chronic post-COVID syndrome: A systematic review and meta-analysis, EClinicalMedicine
Knight, Ho, Pius, Buchan, Carson et al., Stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterization Protocol: Development and validation of the 4-C Mortality Score, BMJ
Kor, Carter, Park, Festic, Banner-Goodspeed et al., Effect of aspirin on development of ARDS in at-risk patients presenting to the emergency department: The LIPS-A randomized clinical trial, JAMA
Kor, Erlich, Gong, Malinchoc, Carter et al., Association of prehospitalization aspirin therapy and acute lung injury: Results of a multicenter international observational study of at-risk patient, Crit. Care Med
Lim, Shin, Nam, Jung, Koo, Proper Management of People with Obesity during the COVID-19 Pandemic, J. Obes. Metab. Syndr
Liu, Blet, Smyth, Li, The science underlying COVID-19: Implications for the cardiovascular system, Circulation
Liu, Zhang, Huang, Yang, Wang et al., -novel Coronavirus (2019-nCoV) Infections Trigger an Exaggerated Cytokine Response Aggravating Lung Injur, Sci. China Life Sci
Mai, Tan, Mainbourg, Potus, Cucherat et al., Venous thromboembolism in COVID-19 compared to non-COVID-19 cohorts: A systematic review with meta-analysis, Vasc. Pharmacol
Mellado-Artigas, Ferreyro, Angriman, Hernández-Sanz, Arruti et al., High-flow nasal oxygen in patients with COVID-19-associated acute respiratory failure, Crit. Care
Miró, Jiménez, Mebazaa, Freund, Burillo-Putze et al., Pulmonary embolism in patients with COVID-19: Incidence, risk factors, clinical characteristics, and outcome, Eur. Heart J
Murata, Kasai, Matsue, Matsumoto, Yatsu et al., Relationship between blood urea nitrogen-to-creatinine ratio at hospital admission and long-term mortality in patients with acute decompensated heart failure, Heart Vessel
Paranjpe, Fuster, Lala, Russak, Glicksberg et al., Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19, J. Am. Coll. Cardiol
Richardson, Hirsch, Narasimhan, Crawford, Mcginn et al., Northwell COVID-19 Research Consortium. Presenting characteristics, comorbidities and outcomes among 5,700 patients hospitalized with COVID-19 in the New York City area, JAMA
Ruan, Yang, Wang, Jiang, Song, Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China, Intensive Care Med
Sattar, Mcinnes, Mcmurray, Obesity Is a Risk Factor Severe COVID-19 Infection: Multiple Potential Mechanisms, Circulation
Sun, Dong, Wang, Xie, Li et al., Characteristics and prognostic factors of disease severity in patients with COVID-19: The Beijing experience, J. Autoimmun
Tan, Mainbourg, Friggeri, Bertoletti, Douplat et al., Arterial and venous thromboembolism in COVID-19: A study-level meta-analysis, Thorax
Wongvibulsin, Garibaldi, Antar, Wen, Wang et al., Development of severe COVID-19 adaptive risk predictor (SCARP), a calculator to predict severe disease or death in hospitalized patients with COVID-19, Ann. Intern. Med, doi:10.7326/m20-6754
Wu, Mcgoogan, Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention, JAMA
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study, Lancet
Zou, Li, Fang, Hu, Bian et al., Acute Physiology and Chronic Health Evaluation II Score as a Predictor of Hospital Mortality in Patients of Coronavirus Disease 2019, Crit. Care Med
DOI record:
{
"DOI": "10.3390/metabo11100679",
"ISSN": [
"2218-1989"
],
"URL": "http://dx.doi.org/10.3390/metabo11100679",
"abstract": "<jats:p>Early identification of patients with COVID-19 who will develop severe or critical disease symptoms is important for delivering proper and early treatment. We analyzed demographic, clinical, immunological, hematological, biochemical and radiographic findings that may be of utility to clinicians in predicting COVID-19 severity and mortality. Electronic medical record data from patients diagnosed with COVID-19 from November 2020 to June 2021 in the COVID-19 Department in the Galilee Medical Center, Nahariya, Israel, were collected. Epidemiologic, clinical, laboratory and imaging variables were analyzed. Multivariate stepwise regression analyses and discriminant analyses were used to identify and validate powerful predictors. The main outcome measure was invasive ventilation, or death. The study population included 390 patients, with a mean age of 61 ± 18, and 51% were male. The non-survivors were mostly male, elderly and overweight and significantly suffered from hypertension, diabetes mellitus type 2, lung disease, hemodialysis and past use of aspirin. Four predictive factors were found that associated with increased disease severity and/or mortality: age, NLR, BUN, and use of high flow oxygen therapy (HFNC). The AUC or diagnostic accuracy was 87%, with a sensitivity of 97%, specificity of 60%, PPV of 87% and NPP of 91%. The cytokine levels of CXCL-10, GCSF, IL-2 and IL-6 were significantly reduced upon the discharge of severely ill COVID-19 patients. The predictive factors associated with increased mortality include age, NLR, BUN, and use of HFNC upon admission. Identifying those with higher risks of mortality could help in early interventions to reduce the risk of death.</jats:p>",
"alternative-id": [
"metabo11100679"
],
"author": [
{
"affiliation": [],
"family": "Basheer",
"given": "Maamoun",
"sequence": "first"
},
{
"affiliation": [],
"family": "Saad",
"given": "Elias",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-7438-5252",
"affiliation": [],
"authenticated-orcid": false,
"family": "Hagai",
"given": "Rechnitzer",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0002-2279-6041",
"affiliation": [],
"authenticated-orcid": false,
"family": "Assy",
"given": "Nimer",
"sequence": "additional"
}
],
"container-title": "Metabolites",
"container-title-short": "Metabolites",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
10,
11
]
],
"date-time": "2021-10-11T05:57:54Z",
"timestamp": 1633931874000
},
"deposited": {
"date-parts": [
[
2021,
10,
21
]
],
"date-time": "2021-10-21T02:11:06Z",
"timestamp": 1634782266000
},
"indexed": {
"date-parts": [
[
2024,
2,
20
]
],
"date-time": "2024-02-20T14:41:33Z",
"timestamp": 1708440093227
},
"is-referenced-by-count": 13,
"issue": "10",
"issued": {
"date-parts": [
[
2021,
10,
2
]
]
},
"journal-issue": {
"issue": "10",
"published-online": {
"date-parts": [
[
2021,
10
]
]
}
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2021,
10,
2
]
],
"date-time": "2021-10-02T00:00:00Z",
"timestamp": 1633132800000
}
}
],
"link": [
{
"URL": "https://www.mdpi.com/2218-1989/11/10/679/pdf",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1968",
"original-title": [],
"page": "679",
"prefix": "10.3390",
"published": {
"date-parts": [
[
2021,
10,
2
]
]
},
"published-online": {
"date-parts": [
[
2021,
10,
2
]
]
},
"publisher": "MDPI AG",
"reference": [
{
"DOI": "10.1001/jama.2020.6775",
"doi-asserted-by": "publisher",
"key": "ref1"
},
{
"DOI": "10.1073/pnas.2004168117",
"doi-asserted-by": "publisher",
"key": "ref2"
},
{
"DOI": "10.1016/S0140-6736(20)30566-3",
"doi-asserted-by": "publisher",
"key": "ref3"
},
{
"DOI": "10.1136/thoraxjnl-2020-215383",
"doi-asserted-by": "publisher",
"key": "ref4"
},
{
"DOI": "10.1016/j.vph.2021.106882",
"doi-asserted-by": "publisher",
"key": "ref5"
},
{
"article-title": "Pulmonary embolism in patients with COVID-19: Incidence, risk factors, clinical characteristics, and outcome",
"author": "Miró",
"first-page": "1148",
"journal-title": "Eur. Heart J.",
"key": "ref6",
"volume": "24",
"year": "2021"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047549",
"doi-asserted-by": "publisher",
"key": "ref7"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047349",
"doi-asserted-by": "publisher",
"key": "ref8"
},
{
"key": "ref9",
"unstructured": "COVID-19 Clinical Management: Living Guidance; 2021. 25 January 2021, COVID-19: Clinical Carehttps://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1"
},
{
"key": "ref10"
},
{
"DOI": "10.1001/jama.2020.2648",
"doi-asserted-by": "publisher",
"key": "ref11"
},
{
"DOI": "10.7326/M20-6754",
"doi-asserted-by": "publisher",
"key": "ref12"
},
{
"DOI": "10.1097/CCM.0000000000004411",
"doi-asserted-by": "publisher",
"key": "ref13"
},
{
"DOI": "10.1016/j.eclinm.2021.100899",
"doi-asserted-by": "publisher",
"key": "ref14"
},
{
"DOI": "10.1007/s00134-020-05991-x",
"doi-asserted-by": "publisher",
"key": "ref15"
},
{
"DOI": "10.1186/s12877-020-01803-5",
"doi-asserted-by": "publisher",
"key": "ref16"
},
{
"DOI": "10.20524/aog.2020.0527",
"doi-asserted-by": "publisher",
"key": "ref17"
},
{
"DOI": "10.1136/bmj.m3339",
"doi-asserted-by": "publisher",
"key": "ref18"
},
{
"DOI": "10.1136/annrheumdis-2020-218323",
"doi-asserted-by": "publisher",
"key": "ref19"
},
{
"DOI": "10.7570/jomes20056",
"doi-asserted-by": "publisher",
"key": "ref20"
},
{
"DOI": "10.1016/S0140-6736(16)30175-1",
"doi-asserted-by": "publisher",
"key": "ref21"
},
{
"DOI": "10.1161/CIRCULATIONAHA.120.047659",
"doi-asserted-by": "publisher",
"key": "ref22"
},
{
"key": "ref23",
"series-title": "Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19)",
"year": "2020"
},
{
"DOI": "10.1016/j.jaut.2020.102473",
"doi-asserted-by": "publisher",
"key": "ref24"
},
{
"DOI": "10.1097/MD.0b013e3181e893ee",
"doi-asserted-by": "publisher",
"key": "ref25"
},
{
"DOI": "10.1016/j.ijcard.2016.04.100",
"doi-asserted-by": "publisher",
"key": "ref26"
},
{
"DOI": "10.1016/j.kint.2020.03.005",
"doi-asserted-by": "publisher",
"key": "ref27"
},
{
"DOI": "10.1007/s00380-018-1135-3",
"doi-asserted-by": "publisher",
"key": "ref28"
},
{
"DOI": "10.1016/S0140-6736(18)30479-3",
"doi-asserted-by": "publisher",
"key": "ref29"
},
{
"DOI": "10.1186/s13054-021-03469-w",
"doi-asserted-by": "publisher",
"key": "ref30"
},
{
"DOI": "10.1007/s11427-020-1643-8",
"doi-asserted-by": "publisher",
"key": "ref31"
},
{
"article-title": "Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely associated with drastically elevated interleukin 6 (IL-6) level in critically ill COVID-19 patients",
"author": "Chen",
"first-page": "ciaa449",
"journal-title": "Clin Infect Dis.",
"key": "ref32",
"volume": "17",
"year": "2020"
},
{
"DOI": "10.1016/j.jacc.2020.05.001",
"doi-asserted-by": "publisher",
"key": "ref33"
},
{
"DOI": "10.1186/s13054-015-0846-4",
"doi-asserted-by": "publisher",
"key": "ref34"
},
{
"DOI": "10.1097/CCM.0000000000000789",
"doi-asserted-by": "publisher",
"key": "ref35"
},
{
"DOI": "10.1378/chest.10-0891",
"doi-asserted-by": "publisher",
"key": "ref36"
},
{
"DOI": "10.1001/jama.2016.6330",
"doi-asserted-by": "publisher",
"key": "ref37"
},
{
"DOI": "10.1097/CCM.0b013e318225757f",
"doi-asserted-by": "publisher",
"key": "ref38"
}
],
"reference-count": 38,
"references-count": 38,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.mdpi.com/2218-1989/11/10/679"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Molecular Biology",
"Biochemistry",
"Endocrinology, Diabetes and Metabolism"
],
"subtitle": [],
"title": "Clinical Predictors of Mortality and Critical Illness in Patients with COVID-19 Pneumonia",
"type": "journal-article",
"volume": "11"
}