Fluvoxamine in the Treatment of Patients with COVID-19
et al., Psychiatry, Psychotherapy and Clinical Psychology, doi:10.34883/PI.2021.12.2.007, Jun 2021
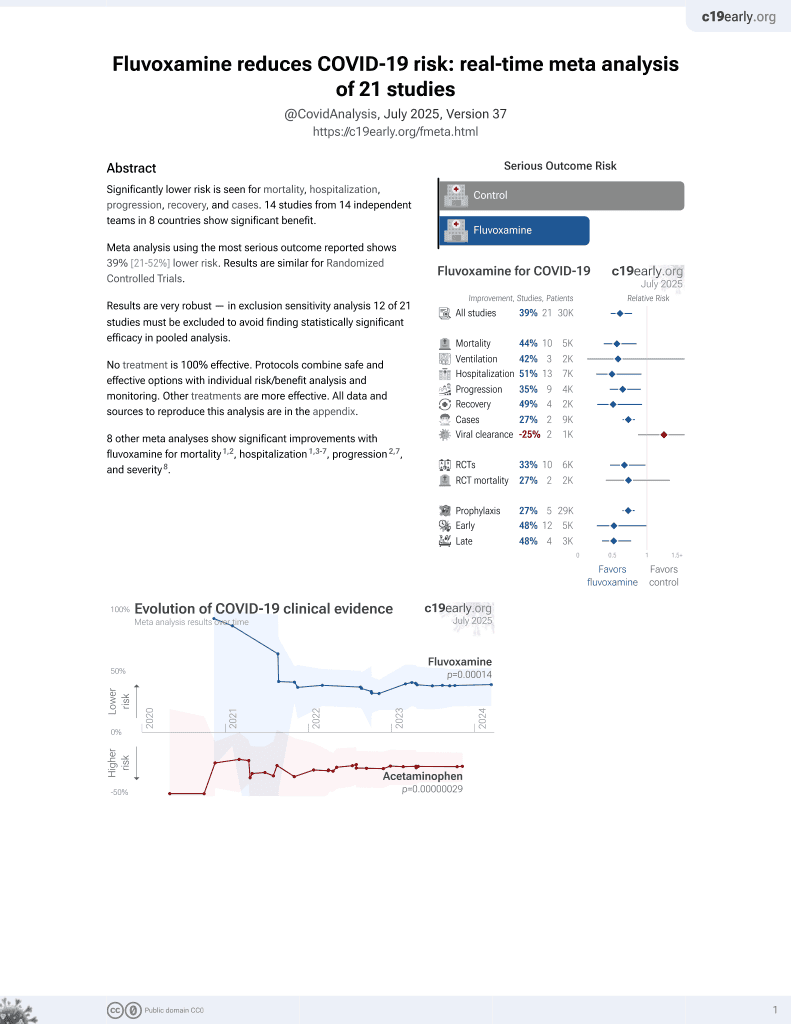
31st treatment shown to reduce risk in
November 2021, now with p = 0.00014 from 21 studies, recognized in 2 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
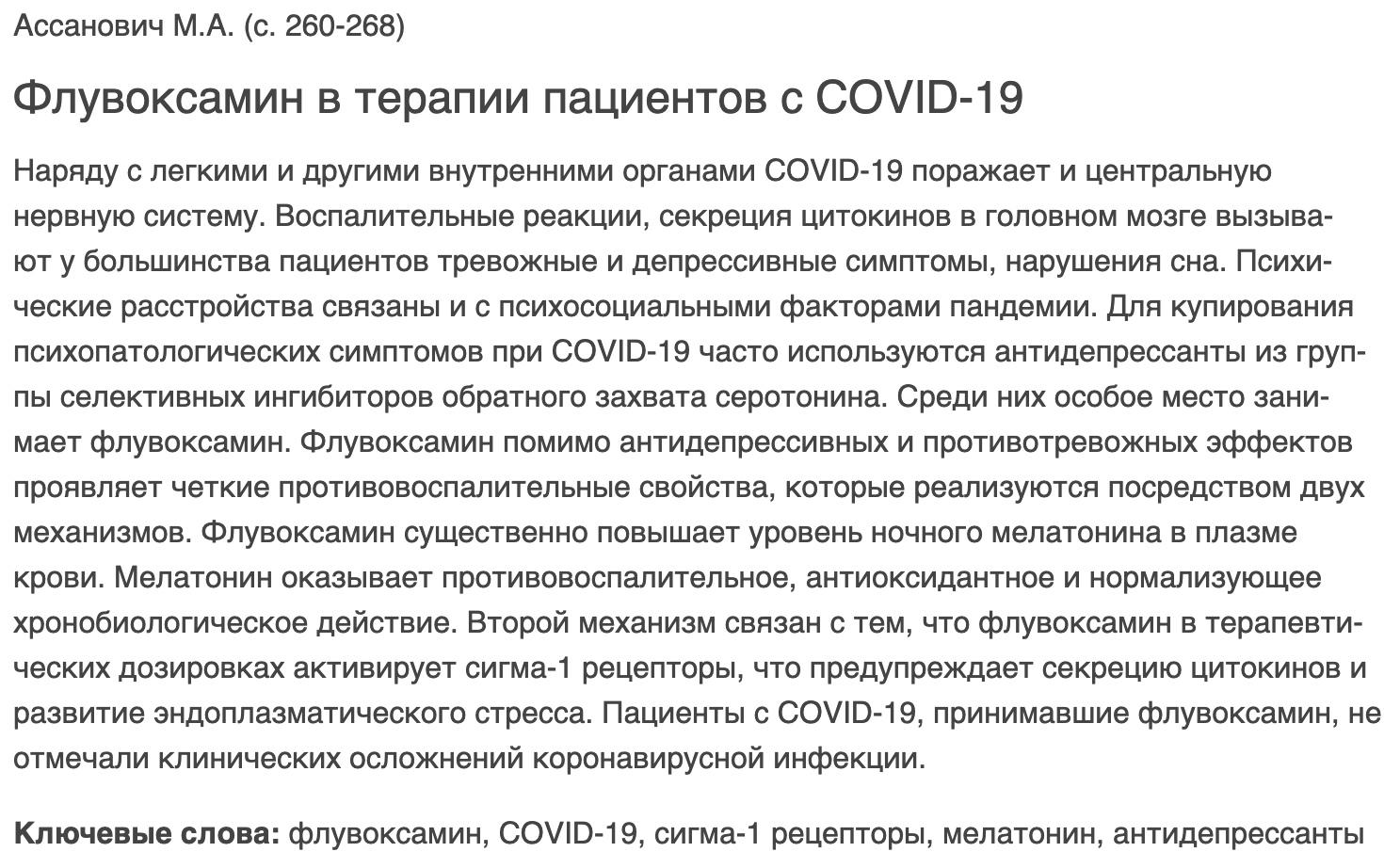
Report on the use of fluvoxamine for COVID-19 noting that "patients with COVID-19 taking fluvoxamine did not report clinical complications of coronavirus infection". Only the abstract is currently available.
Assanovich et al., 29 Jun 2021, peer-reviewed, 1 author.
DOI record:
{
"DOI": "10.34883/pi.2021.12.2.007",
"ISSN": [
"2220-1122",
"2414-2212"
],
"URL": "http://dx.doi.org/10.34883/PI.2021.12.2.007",
"abstract": "<jats:p>Наряду с легкими и другими внутренними органами COVID-19 поражает и центральную нервную систему. Воспалительные реакции, секреция цитокинов в головном мозге вызывают у большинства пациентов тревожные и депрессивные симптомы, нарушения сна. Психические расстройства связаны и с психосоциальными факторами пандемии. Для купирования психопатологических симптомов при COVID-19 часто используются антидепрессанты из группы селективных ингибиторов обратного захвата серотонина. Среди них особое место занимает флувоксамин. Флувоксамин помимо антидепрессивных и противотревожных эффектов проявляет четкие противовоспалительные свойства, которые реализуются посредством двух механизмов. Флувоксамин существенно повышает уровень ночного мелатонина в плазме крови. Мелатонин оказывает противовоспалительное, антиоксидантное и нормализующее хронобиологическое действие. Второй механизм связан с тем, что флувоксамин в терапевтических дозировках активирует сигма-1 рецепторы, что предупреждает секрецию цитокинов и развитие эндоплазматического стресса. Пациенты с COVID-19, принимавшие флувоксамин, не отмечали клинических осложнений коронавирусной инфекции.</jats:p>\n <jats:p>COVID-19 affects central nervous system along with lungs and other internal organs. Inflammatory reactions, secretion of cytokines in brain cause anxiety and depressive symptoms, sleep disturbances in most patients. Mental disorders are also associated with psychosocial factors of the pandemic. SSRI antidepressants are often used to relieve psychopathological symptoms in COVID-19. Among them, fluvoxamine occupies a special place. Fluvoxamine, in addition to antidepressant and anti-anxiety effects, exhibits clear anti-inflammatory properties, which are realized through two mechanisms. Fluvoxamine significantly increases the level of nocturnal melatonin in blood plasma. Melatonin has anti-inflammatory, antioxidant and chronobiological normalizing effects. The second mechanism is associated with the fact that fluvoxamine in therapeutic dosages activates sigma-1 receptors, which prevents secretion of cytokines and development of endoplasmic stress. Patients with COVID-19 taking fluvoxamine did not report clinical complications of coronavirus infection.</jats:p>",
"author": [
{
"affiliation": [],
"family": "Ассанович",
"given": "М.А.",
"sequence": "first"
}
],
"container-title": "Психиатрия, психотерапия и клиническая психология",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
2,
24
]
],
"date-time": "2022-02-24T10:40:46Z",
"timestamp": 1645699246000
},
"deposited": {
"date-parts": [
[
2022,
2,
24
]
],
"date-time": "2022-02-24T10:42:00Z",
"timestamp": 1645699320000
},
"indexed": {
"date-parts": [
[
2022,
4,
2
]
],
"date-time": "2022-04-02T05:29:54Z",
"timestamp": 1648877394484
},
"is-referenced-by-count": 0,
"issue": "2",
"issued": {
"date-parts": [
[
2021,
6,
4
]
]
},
"journal-issue": {
"issue": "2",
"published-print": {
"date-parts": [
[
2021,
6,
4
]
]
}
},
"language": "ru",
"member": "34055",
"original-title": [
"Флувоксамин в терапии пациентов с COVID-19"
],
"page": "260-268",
"prefix": "10.34883",
"published": {
"date-parts": [
[
2021,
6,
4
]
]
},
"published-print": {
"date-parts": [
[
2021,
6,
4
]
]
},
"publisher": "Professionals Publications",
"reference": [
{
"DOI": "10.1093/qjmed/hcaa110",
"doi-asserted-by": "crossref",
"key": "1",
"unstructured": "Cullen W., Gulati G., Kelly B.D. (2020) Mental health in the COVID-19 pandemic. QJM : monthly journal of the Association of Physicians, vol. 113, no 5, pp. 311–312."
},
{
"DOI": "10.1007/s10072-020-04544-w",
"doi-asserted-by": "crossref",
"key": "2",
"unstructured": "Orsini A., Corsi M., Santangelo A., Riva A. (2020) Challenges and management of neurological and psychiatric manifestations in SARS-CoV-2 (COVID-19) patients. Neurological Sciences, vol. 41, pp. 2353–2366."
},
{
"DOI": "10.1177/1073858420967892",
"doi-asserted-by": "crossref",
"key": "3",
"unstructured": "Bouças A.P., Rheinheimer J., Lagopoulos J. (2020) Why Severe COVID-19 Patients Are at Greater Risk of Developing Depression: A Molecular Perspective. Neuroscientist (electronic journal). Available at: https://journals.sagepub.com/doi/10.1177/1073858420967892?url_ver=Z39.88- 2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed (accesed 5 May 2021)."
},
{
"DOI": "10.1016/j.pnpbp.2004.11.003",
"doi-asserted-by": "crossref",
"key": "4",
"unstructured": "Schiepers O.J.G., Wichers M.C., Maes M. (2005) Cytokines and major depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry, vol. 29, pp. 201–217."
},
{
"DOI": "10.1016/j.drudis.2020.06.022",
"doi-asserted-by": "crossref",
"key": "5",
"unstructured": "Villoutreix B.O., Beaune P.H., Tamouza R. (2020) Prevention of COVID-19 by drug repurposing: rationale from drugs prescribed for mental disorders. Drug Discovery Today, vol. 25, pp.1287–1290."
},
{
"DOI": "10.1111/fcp.12586",
"doi-asserted-by": "crossref",
"key": "6",
"unstructured": "Lemaitre F., Solas C., Grégoire M. (2020) Potential drug–drug interactions associated with drugs currently proposed for COVID-19 treatment in patients receiving other treatments. Fundamental and Clinical Pharmacology, vol. 34, pp. 530–547."
},
{
"DOI": "10.1177/2045125320935306",
"doi-asserted-by": "crossref",
"key": "7",
"unstructured": "Bishara D., Kalafatis C., Taylor D. (2020) Emerging and experimental treatments for COVID-19 and drug interactions with psychotropic agents. Therapeutic Advances in Psychopharmacology (electronic journal), vol. 10. Available at: https://journals.sagepub.com/doi/ full/10.1177/2045125320935306 (Accessed 5 May 2021)."
},
{
"DOI": "10.1192/bjp.2020.84",
"doi-asserted-by": "crossref",
"key": "8",
"unstructured": "Zhang K., Zhou X., Liu H. (2021) Treatment concerns for psychiatric symptoms in patients with COVID-19 with or without psychiatric disorders. British Journal of Psychiatry, vol. 217, pp. 351."
},
{
"DOI": "10.1007/s00406-020-01231-x",
"doi-asserted-by": "crossref",
"key": "9",
"unstructured": "Hashimoto K. (2021) Repurposing of CNS drugs to treat COVID-19 infection: targeting the sigma-1 receptor. European Archives of Psychiatry and Clinical Neuroscience, vol. 271, pp. 249–258."
},
{
"DOI": "10.4103/jfmpc.jfmpc_513_20",
"doi-asserted-by": "crossref",
"key": "10",
"unstructured": "Rohilla J., Tak P., Jhanwar S. (2020) Primary care physician’s approach for mental health impact of COVID-19. Journal of Family Medicine and Primary Care (electronic journal), vol. 9. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7567264/ (Accessed 5 May 2021)."
},
{
"DOI": "10.1016/j.intimp.2015.06.031",
"doi-asserted-by": "crossref",
"key": "11",
"unstructured": "Park E.J., Lee J.H., Jeong D.C. (2015) Natural killer cell activity in patients with major depressive disorder treated with escitalopram. International Immunopharmacology, vol. 28, pp. 409–413."
},
{
"DOI": "10.1002/14651858.CD006114.pub2",
"doi-asserted-by": "crossref",
"key": "12",
"unstructured": "Omori I.M., Watanabe N., Nakagawa A. (2010) Fluvoxamine versus other anti-depressive agents for depression. Cochrane Database of Systematic Reviews. Available at: https://www.cochrane.org/CD006114/DEPRESSN_fluvoxamine-versus-other-anti-depressive-agents-for- depression#:~:text=Fluvoxamine versus other anti-depressive agents for depression Major,symptoms%2C inappropriate guilt and morbid thoughts of death (Accessed 5 May 2021)."
},
{
"key": "13",
"unstructured": "Irons J. (2005) Fluvoxamine in the treatment of anxiety disorders. Neuropsychiatric disease and treatment, vol. 1, pp. 289–299."
},
{
"DOI": "10.1016/j.lfs.2020.117583",
"doi-asserted-by": "crossref",
"key": "14",
"unstructured": "Zhang R., Wang X., Ni L. (2020) COVID-19: Melatonin as a potential adjuvant treatment. Life Sciences (electronic journal). Available at: https://www. sciencedirect.com/science/article/abs/pii/S0024320520303313 (Accessed 5 May 2021)."
},
{
"DOI": "10.1080/08830185.2020.1756284",
"doi-asserted-by": "crossref",
"key": "15",
"unstructured": "Shneider A., Kudriavtsev A., Vakhrusheva A. (2020) Can melatonin reduce the severity of COVID-19 pandemic? International Reviews of Immunology, vol. 39, pp. 153–162."
},
{
"DOI": "10.1111/jpi.12683",
"doi-asserted-by": "crossref",
"key": "16",
"unstructured": "Acuña-Castroviejo D., Escames G., Figueira J.C. (2020) Clinical trial to test the efficacy of melatonin in COVID-19. Journal of Pineal Research, vol. 69, pp. 1–4."
},
{
"DOI": "10.3389/fmed.2020.00226",
"doi-asserted-by": "crossref",
"key": "17",
"unstructured": "Reiter R.J., Abreu-Gonzalez P., Marik P.E. (2020) Therapeutic Algorithm for Use of Melatonin in Patients With COVID-19. Frontiers in Medicine, vol. 7. Available at: https://www.frontiersin.org/articles/10.3389/fmed.2020.00226/full (Accessed 5 May 2021)."
},
{
"DOI": "10.1007/s002280050729",
"doi-asserted-by": "crossref",
"key": "18",
"unstructured": "Von Bahr C., Ursing C., Yasui N. (2000) Fluvoxamine but not citalopram increases serum melatonin in healthy subjects – An indication that cytochrome P450 CYP1A2 and CYP2C19 hydroxylate melatonin. European Journal of Clinical Pharmacology, vol. 56, pp. 123–127."
},
{
"DOI": "10.1007/s00213-020-05753-z",
"doi-asserted-by": "crossref",
"key": "19",
"unstructured": "Anderson G.M. (2021) Fluvoxamine, melatonin and COVID-19. Psychopharmacology, vol. 238, no 2, pp. 611."
},
{
"DOI": "10.1016/j.bbr.2016.08.005",
"doi-asserted-by": "crossref",
"key": "20",
"unstructured": "Dallé E., Daniels W.M.U., Mabandla M V. (2017) Fluvoxamine maleate normalizes striatal neuronal inflammatory cytokine activity in a Parkinsonian rat model associated with depression. Behavioural Brain Research, vol. 316, pp. 189–196."
},
{
"DOI": "10.2147/NDT.S123121",
"doi-asserted-by": "crossref",
"key": "21",
"unstructured": "Yoshimura R., Katsuki A., Atake K. (2017) Influence of fluvoxamine on plasma interleukin-6 or clinical improvement in patients with major depressive disorder. Neuropsychiatric Disease and Treatment, vol. 13, pp. 437–441."
},
{
"DOI": "10.22541/au.159335613.31156244",
"doi-asserted-by": "crossref",
"key": "22",
"unstructured": "Troncone L.R. (2020) COVID-19, cytokine storm and sigma-1 receptors: potential treatments at hand? Authorea, vol. 19, pp. 1–3."
},
{
"DOI": "10.1002/hup.1106",
"doi-asserted-by": "crossref",
"key": "23",
"unstructured": "Hindmarch I., Hashimoto K. (2010) Cognition and depression: The effects of fluvoxamine, a sigma-1 receptor agonist, reconsidered. Human Psychopharmacology, vol. 25, pp. 193–200."
},
{
"DOI": "10.1001/jama.2020.22760",
"doi-asserted-by": "crossref",
"key": "24",
"unstructured": "Lenze E.J., Mattar C., Zorumski C.F. (2020) Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients with Symptomatic COVID-19: A Randomized Clinical Trial. Journal of the American Medical Association, vol. 324, pp. 2292–2300."
},
{
"DOI": "10.1093/ofid/ofab050",
"doi-asserted-by": "crossref",
"key": "25",
"unstructured": "Seftel D., Boulware D.R. (2021) Prospective Cohort of Fluvoxamine for Early Treatment of Coronavirus Disease 19. Open Forum Infectious Diseases, vol. 8, pp. 1–3."
}
],
"reference-count": 25,
"references-count": 25,
"relation": {},
"resource": {
"primary": {
"URL": "https://psihea.recipe.by/ru/?editions=2021-tom-12-n-2&group_id=item_1&article_id=line_1"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Fluvoxamine in the Treatment of Patients with COVID-19",
"type": "journal-article"
}