The Influence of Physical Activity on COVID-19 Prevention Among Quarantined Individuals: A Case–Control Study
et al., Journal of Multidisciplinary Healthcare, doi:10.2147/JMDH.S352753, Feb 2022
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 142 patients in Saudi Arabia, showing no significant difference in cases with physical activity.
|
risk of case, 5.7% lower, RR 0.94, p = 0.85, high activity levels 35 of 71 (49.3%), low activity levels 38 of 71 (53.5%), NNT 24, adjusted per study, odds ratio converted to relative risk, multivariable.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Almansour et al., 17 Feb 2022, retrospective, Saudi Arabia, peer-reviewed, 12 authors, study period April 2020 - June 2020.
Contact: ahmansour@iau.edu.sa.
The Influence of Physical Activity on COVID-19 Prevention Among Quarantined Individuals: A Case–Control Study
Journal of Multidisciplinary Healthcare, doi:10.2147/jmdh.s352753
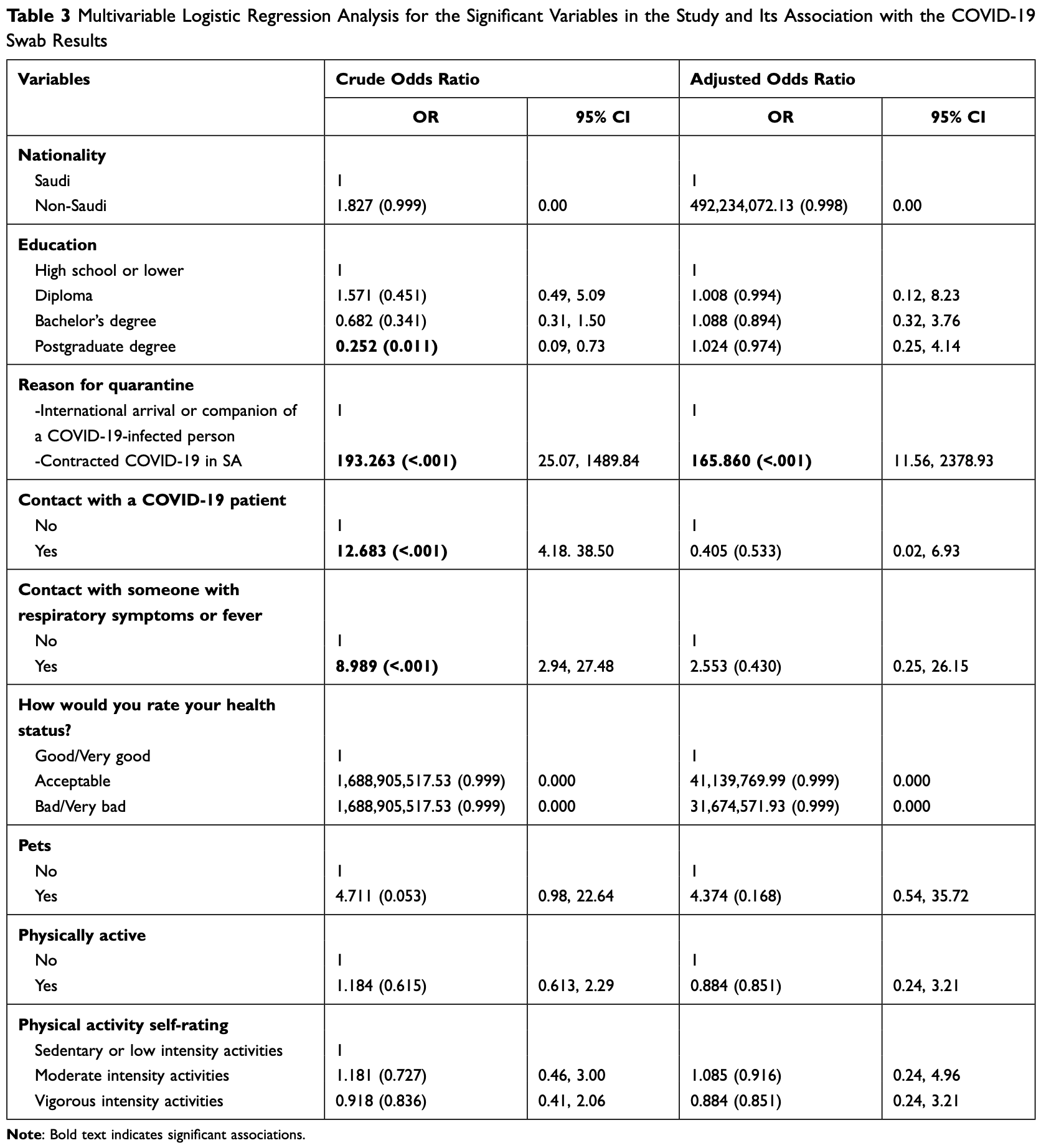
Background: Physical activity is a known preventive measure for many worldwide public health issues. The purpose of this study is to assess the association between physical activity and the susceptibility to COVID-19 infection. Patients and Methods: This was a retrospective matched case-control study involving adult participants quarantined with IAU, Dammam, Saudi Arabia. The total randomized sample of study participants were 142, in which 73 of them were tested positive for COVID-19 test and matched for both age and sex with their respective healthy controls who tested negative for COVID-19 test to determine the risk associated with that exposure. Results: Several variables are assessed regarding their influence on the susceptibility of COVID-19 infection. Exactly half indicated that they were physically active (n = 71). Physical activity did not show any significant association with COVID-19 contraction (x 2 = 0.254, P= 0.614) nor self-rated level of physical activity (x 2 = 0.122, P= 0.727). Less than half of the participants who had contact with a COVID-19 patient within 14 days of admission to quarantine appeared to have a significantly higher incidence of positive COVID-19 swab results compared to those who did not (x 2 = 27.121, P= <0.001). While third of the participants who indicated that they have had a contact with someone who have Respiratory symptoms or fever within 14 days before admission were tested positive for COVID-19. Participants with lower educational degrees are more likely to be infected with COVID-19. While the rest of the demographic variables appear to be not significantly related to the likelihood of being COVID-19 infected, these include gender, marital status, employment status, age, and BMI.
Conclusion: The present study showed no significant association between physical activity and susceptibility to COVID-19 infection. We recommend a larger sample size to further clarify the relationship between other variables and susceptibility of COVID-19.
Ethics Approval and Informed Consent Ethical approval is obtained from the Institutional Review Board in Imam Abdulrahman bin Faisal university (IRB-UGS-2021-01-154). Participants were asked to verbally consent to participate in the study prior to their participation.
Consent for Publication The corresponding author on behalf of the coauthors in the study would like to provide the journal their consent to publish the manuscript.
Author Contributions All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding No funding was relevant to this project.
Disclosure The authors report no conflicts of interest in this work.
References
Burke, Midgley, Dratch, Active monitoring of persons exposed to patients with confirmed COVID-19 -United States, January-February 2020, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm6909e1
Busetto, Bettini, Fabris, Obesity and COVID-19: an Italian snapshot, Obesity, doi:10.1002/oby.22918
Cetron, Landwirth, Public health and ethical considerations in planning for quarantine, Yale J Biol Med
Cetron, Simone, Battling 21st-century scourges with a 14th-century toolbox, Emerg Infect Dis, doi:10.3201/eid1011.040797_12
Chan, Yuan, Kok, A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster, Lancet, doi:10.1016/S0140-6736(20)30154-9
Chen, Deng, Chen, Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: a cross-sectional study, Acta Ophthalmol, doi:10.1111/aos.14472
Chirico, Lucidi, Galli, COVID-19 outbreak and physical activity in the Italian population: a cross-sectional analysis of the underlying psychosocial mechanisms, Front Psychol
Codella, Chirico, Lucidi, Ferrulli, Torre et al., The immune-modulatory effects of exercise should be favorably harnessed against COVID-19, J Endocrinol Invest, doi:10.1007/s40618-020-01403-5
Da Silveira, Da, Fagundes, Bizuti, Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature, Clin Exp Med
Da Silveira, Da, Fagundes, Bizuti, Starck et al., Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature, Clin Exp Med, doi:10.1007/s10238-020-00650-3
Dixon, Peters, The effect of obesity on lung function, Expet Rev Respir Med
Goh, Cutter, Heng, Epidemiology and control of SARS in Singapore, Ann Acad Med Singapore
Goumenou, Sarigiannis, Tsatsakis, COVID-19 in Northern Italy: an integrative overview of factors possibly influencing the sharp increase of the outbreak, Mol Med Rep
Huang, Wang, Li, Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China, Lancet, doi:10.1016/S0140-6736(20)30183-5
Hussain, Mahawar, Xia, Yang, El-Hasani, Obesity and mortality of COVID-19. meta-analysis, Obes Res Clin Pract, doi:10.1016/j.orcp.2020.07.002
Kassir, Risk of COVID-19 for patients with obesity, Obes Rev, doi:10.1111/obr.13034
Kulcsar, Coleman, Beck, Frieman, Comorbid diabetes results in immune dysregulation and enhanced disease severity following MERS-CoV infection, JCI Insight, doi:10.1172/jci.insight.131774
Kwok, Adam, Ho, Obesity: a critical risk factor in the COVID-19 pandemic, Multidisciplinary Healthcare, doi:10.1111/cob.12403
Li, Guan, Wu, Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia, N Engl J Med, doi:10.1056/NEJMoa2001316
Liu, Liao, Qian, Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020, Emerg Infect Dis, doi:10.3201/eid2606.200239
López-Bueno, Calatayud, Andersen, Cardiorespiratory fitness in adolescents before and after the COVID-19 confinement: a prospective cohort study, Eur J Pediatr, doi:10.1007/s00431-021-04029-8
López-Bueno, Calatayud, Andersen, Immediate impact of the COVID-19 confinement on physical activity levels in Spanish adults, Sustainability, doi:10.3390/su12145708
Margolis, Educational differences in healthy behavior changes and adherence among middle-aged Americans, J Health Soc Behav, doi:10.1177/0022146513489312
Maugeri, Castrogiovanni, Battaglia, The impact of physical activity on psychological health during Covid-19 pandemic in Italy, Heliyon, doi:10.1016/j.heliyon.2020.e04315
Moser, Galindo-Fraga, Ortiz-Hernandez, Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses, Influenza Respir Viruses
Nieman, Wentz, The compelling link between physical activity and the body's defense system, J Sport Health Sci, doi:10.1016/j.jshs.2018.09.009
Renzo, Gualtieri, Pivari, Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey, J Transl Med, doi:10.1186/s12967-020-02399-5
Scarinci, Pandya, Kim, Factors associated with perceived susceptibility to COVID-19 among urban and rural adults in Alabama, J Commun Health, doi:10.1007/s10900-021-00976-3
Soeroto, Soetedjo, Purwiga, Effect of increased BMI and obesity on the outcome of COVID-19 adult patients: a systematic review and meta-analysis, Diabetes Metab Syndr, doi:10.1016/j.dsx.2020.09.029
Tian, Hu, Lou, Characteristics of COVID-19 infection in Beijing, J Hosp Infect, doi:10.1016/j.jinf.2020.02.018
Tornaghi, Lovecchio, Vandoni, Chirico, Codella, Physical activity levels across COVID-19 outbreak in youngsters of Northwestern Lombardy, J Sports Med Phys Fitness, doi:10.23736/S0022-4707.20.11600-1
Wen, Wu, Stressing harms of physical inactivity to promote exercise, Lancet, doi:10.1016/S0140-6736(12)60954-4
Wilder-Smith, Freedman, Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak, J Travel Med, doi:10.1093/jtm/taaa020
DOI record:
{
"DOI": "10.2147/jmdh.s352753",
"ISSN": [
"1178-2390"
],
"URL": "http://dx.doi.org/10.2147/JMDH.S352753",
"author": [
{
"affiliation": [],
"family": "Almansour",
"given": "Abdulelah",
"sequence": "first"
},
{
"affiliation": [],
"family": "Alagil",
"given": "Jumana",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alamoudi",
"given": "Naela B",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alamrie",
"given": "Rahmah M",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alarifi",
"given": "Sundus",
"sequence": "additional"
},
{
"affiliation": [],
"family": "AlUrifan",
"given": "Sarah",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-7924-0004",
"affiliation": [],
"authenticated-orcid": true,
"family": "Althunyan",
"given": "Abdullatif",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alghumlas",
"given": "Abdullah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Alreedy",
"given": "Abdullah",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Aldhawyan",
"given": "Adam",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6502-6402",
"affiliation": [],
"authenticated-orcid": true,
"family": "Alshehri",
"given": "Shaher",
"sequence": "additional"
},
{
"ORCID": "http://orcid.org/0000-0001-6454-3678",
"affiliation": [],
"authenticated-orcid": true,
"family": "Alumran",
"given": "Arwa",
"sequence": "additional"
}
],
"container-title": "Journal of Multidisciplinary Healthcare",
"container-title-short": "JMDH",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2022,
2,
16
]
],
"date-time": "2022-02-16T15:20:24Z",
"timestamp": 1645024824000
},
"deposited": {
"date-parts": [
[
2022,
2,
16
]
],
"date-time": "2022-02-16T15:20:35Z",
"timestamp": 1645024835000
},
"indexed": {
"date-parts": [
[
2022,
4,
4
]
],
"date-time": "2022-04-04T05:54:09Z",
"timestamp": 1649051649277
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2022,
2
]
]
},
"language": "en",
"license": [
{
"URL": "http://creativecommons.org/licenses/by-nc/3.0/",
"content-version": "unspecified",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
2,
1
]
],
"date-time": "2022-02-01T00:00:00Z",
"timestamp": 1643673600000
}
}
],
"link": [
{
"URL": "https://www.dovepress.com/getfile.php?fileID=78363",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://www.dovepress.com/getfile.php?fileID=78363",
"content-type": "application/pdf",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "301",
"original-title": [],
"page": "271-280",
"prefix": "10.2147",
"published": {
"date-parts": [
[
2022,
2
]
]
},
"published-online": {
"date-parts": [
[
2022,
2
]
]
},
"publisher": "Informa UK Limited",
"reference": [
{
"key": "ref1",
"unstructured": "World Health Organization. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-Ncov). Geneva, Switzerland: World Health Organization; 2020."
},
{
"key": "ref2",
"unstructured": "World Health Organization. Coronavirus disease (COVID-19) – events as they happen [webpage]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Accessed June 14, 2020."
},
{
"DOI": "10.1093/jtm/taaa020",
"author": "Wilder-Smith",
"doi-asserted-by": "publisher",
"journal-title": "J Travel Med",
"key": "ref3",
"volume": "27",
"year": "2020"
},
{
"key": "ref4",
"unstructured": "Government of Saudi Arabia. COVID-19 dashboard: Saudi Arabia [webpage]. Available from: https://covid19.moh.gov.sa/. Accessed June 14, 2020."
},
{
"key": "ref5",
"unstructured": "Kingdom of Saudi Arabia. Measures in response to COVID [webpage]. Available from: https://home.kpmg/xx/en/home/insights/2020/04/saudi-arabia-government-and-institution-measures-in-response-to-covid.html. Accessed June 14, 2020."
},
{
"author": "Goumenou",
"first-page": "20",
"journal-title": "Mol Med Rep",
"key": "ref6",
"volume": "22",
"year": "2020"
},
{
"DOI": "10.3201/eid1011.040797_12",
"author": "Cetron",
"doi-asserted-by": "publisher",
"first-page": "2053",
"journal-title": "Emerg Infect Dis",
"key": "ref7",
"volume": "10",
"year": "2004"
},
{
"author": "Goh",
"first-page": "301",
"journal-title": "Ann Acad Med Singapore",
"key": "ref8",
"volume": "35",
"year": "2006"
},
{
"author": "Cetron",
"first-page": "325",
"journal-title": "Yale J Biol Med",
"key": "ref9",
"volume": "78",
"year": "2005"
},
{
"DOI": "10.3390/su12145708",
"author": "López-Bueno",
"doi-asserted-by": "publisher",
"first-page": "5708",
"journal-title": "Sustainability",
"key": "ref10",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.3389/fpsyg.2020.02100",
"author": "Chirico",
"doi-asserted-by": "crossref",
"first-page": "2100",
"journal-title": "Front Psychol",
"key": "ref11",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.23736/S0022-4707.20.11600-1",
"author": "Tornaghi",
"doi-asserted-by": "publisher",
"first-page": "971",
"journal-title": "J Sports Med Phys Fitness",
"key": "ref12",
"volume": "61",
"year": "2021"
},
{
"DOI": "10.1016/j.jshs.2018.09.009",
"author": "Nieman",
"doi-asserted-by": "publisher",
"first-page": "201",
"journal-title": "J Sport Health Sci",
"key": "ref13",
"volume": "8",
"year": "2019"
},
{
"DOI": "10.1007/s10238-020-00650-3",
"author": "da Silveira",
"doi-asserted-by": "publisher",
"first-page": "15",
"journal-title": "Clin Exp Med",
"key": "ref14",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1007/s40618-020-01403-5",
"author": "Codella",
"doi-asserted-by": "publisher",
"first-page": "1119",
"journal-title": "J Endocrinol Invest",
"key": "ref15",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.1016/S0140-6736(12)60954-4",
"author": "Wen",
"doi-asserted-by": "publisher",
"first-page": "192",
"journal-title": "Lancet",
"key": "ref16",
"volume": "380",
"year": "2012"
},
{
"key": "ref17",
"unstructured": "IBM Corp. IBM SPSS Statistics for Windows (Version 19.0). Armonk, NY: IBM Corp; 2010."
},
{
"DOI": "10.1016/j.heliyon.2020.e04315",
"author": "Maugeri",
"doi-asserted-by": "publisher",
"first-page": "e04315",
"journal-title": "Heliyon",
"key": "ref18",
"volume": "6",
"year": "2020"
},
{
"author": "da Silveira",
"first-page": "15",
"journal-title": "Clin Exp Med",
"key": "ref19",
"volume": "2021",
"year": "2020"
},
{
"DOI": "10.1007/s10900-021-00976-3",
"author": "Scarinci",
"doi-asserted-by": "publisher",
"first-page": "932",
"journal-title": "J Commun Health",
"key": "ref20",
"volume": "46",
"year": "2021"
},
{
"DOI": "10.1177/0022146513489312",
"author": "Margolis",
"doi-asserted-by": "publisher",
"first-page": "353",
"journal-title": "J Health Soc Behav",
"key": "ref21",
"volume": "54",
"year": "2013"
},
{
"DOI": "10.3201/eid2606.200239",
"author": "Liu",
"doi-asserted-by": "publisher",
"journal-title": "Emerg Infect Dis",
"key": "ref22",
"volume": "26",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30154-9",
"author": "Chan",
"doi-asserted-by": "publisher",
"first-page": "514",
"journal-title": "Lancet",
"key": "ref23",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.1056/NEJMoa2001316",
"author": "Li",
"doi-asserted-by": "publisher",
"first-page": "1199",
"journal-title": "N Engl J Med",
"key": "ref24",
"volume": "382",
"year": "2020"
},
{
"DOI": "10.1016/S0140-6736(20)30183-5",
"author": "Huang",
"doi-asserted-by": "publisher",
"first-page": "497",
"journal-title": "Lancet",
"key": "ref25",
"volume": "395",
"year": "2020"
},
{
"DOI": "10.15585/mmwr.mm6909e1",
"author": "Burke",
"doi-asserted-by": "publisher",
"first-page": "245",
"journal-title": "MMWR Morb Mortal Wkly Rep",
"key": "ref26",
"volume": "69",
"year": "2020"
},
{
"DOI": "10.1016/j.jinf.2020.02.018",
"author": "Tian",
"doi-asserted-by": "publisher",
"first-page": "401",
"journal-title": "J Hosp Infect",
"key": "ref27",
"volume": "80",
"year": "2020"
},
{
"DOI": "10.1111/aos.14472",
"author": "Chen",
"doi-asserted-by": "publisher",
"first-page": "951",
"journal-title": "Acta Ophthalmol",
"key": "ref28",
"volume": "98",
"year": "2020"
},
{
"key": "ref29",
"unstructured": "World Health Organization. Health topics [webpage]. Available from: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed December 5, 2021."
},
{
"DOI": "10.1016/j.dsx.2020.09.029",
"author": "Soeroto",
"doi-asserted-by": "publisher",
"first-page": "1897",
"journal-title": "Diabetes Metab Syndr",
"key": "ref30",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1007/s00431-021-04029-8",
"author": "López-Bueno",
"doi-asserted-by": "publisher",
"first-page": "2287",
"journal-title": "Eur J Pediatr",
"key": "ref31",
"volume": "180",
"year": "2021"
},
{
"DOI": "10.1111/obr.13034",
"author": "Kassir",
"doi-asserted-by": "publisher",
"first-page": "e13034",
"journal-title": "Obes Rev",
"key": "ref32",
"volume": "21",
"year": "2020"
},
{
"author": "Moser",
"first-page": "3e9",
"journal-title": "Influenza Respir Viruses",
"key": "ref33",
"volume": "13",
"year": "2019"
},
{
"DOI": "10.1002/oby.22918",
"author": "Busetto",
"doi-asserted-by": "publisher",
"first-page": "1600",
"journal-title": "Obesity",
"key": "ref34",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.1016/j.orcp.2020.07.002",
"author": "Hussain",
"doi-asserted-by": "publisher",
"first-page": "295",
"journal-title": "Obes Res Clin Pract",
"key": "ref35",
"volume": "14",
"year": "2020"
},
{
"DOI": "10.1186/s12967-020-02399-5",
"author": "Di Renzo",
"doi-asserted-by": "publisher",
"first-page": "1",
"journal-title": "J Transl Med",
"key": "ref36",
"volume": "18",
"year": "2020"
},
{
"DOI": "10.1172/jci.insight.131774",
"author": "Kulcsar",
"doi-asserted-by": "publisher",
"journal-title": "JCI Insight",
"key": "ref37",
"volume": "4",
"year": "2019"
},
{
"author": "Dixon",
"first-page": "755e67",
"journal-title": "Expet Rev Respir Med",
"key": "ref38",
"volume": "12",
"year": "2018"
},
{
"DOI": "10.1111/cob.12403",
"author": "Kwok",
"doi-asserted-by": "publisher",
"first-page": "e12403",
"journal-title": "Clin Obes",
"key": "ref39",
"volume": "10",
"year": "2020"
}
],
"reference-count": 39,
"references-count": 39,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.dovepress.com/the-influence-of-physical-activity-on-covid-19-prevention-among-quaran-peer-reviewed-fulltext-article-JMDH"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Medicine",
"General Nursing"
],
"subtitle": [],
"title": "The Influence of Physical Activity on COVID-19 Prevention Among Quarantined Individuals: A Case–Control Study",
"type": "journal-article",
"volume": "Volume 15"
}
