The potential therapeutic effect of metformin in type 2 diabetic patients with severe COVID-19
et al., European Review for Medical and Pharmacological Sciences, doi:10.26355/eurrev_202312_34583, Dec 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
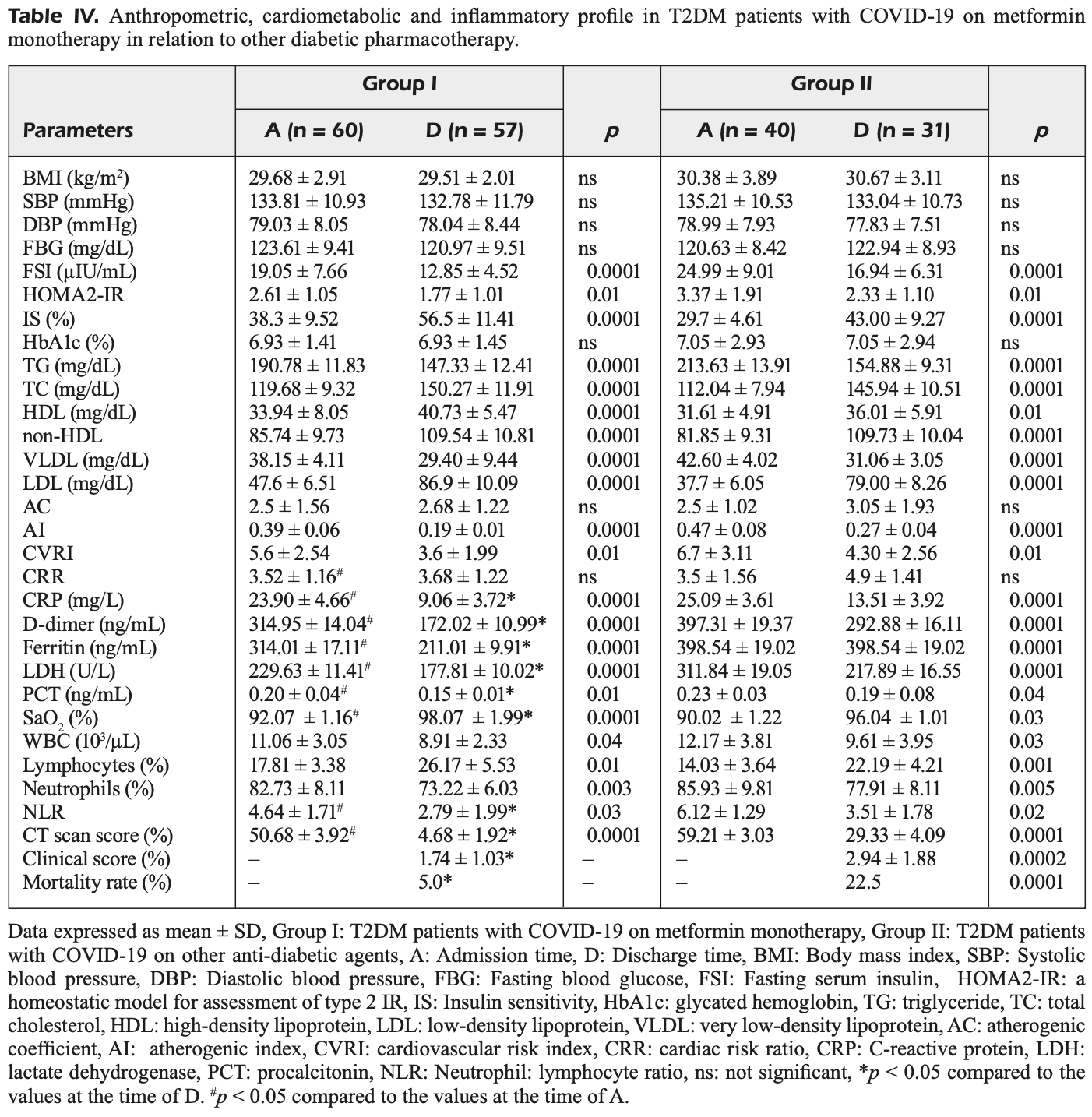
Prospective study of 60 hospitalized type 2 diabetes patients with COVID-19 on metformin monotherapy compared to 40 patients on other diabetes treatments, showing significantly lower inflammatory biomarkers, oxidative stress, and mortality, and improvements in radiological and clinical outcomes with metformin. Confounding due to differences in baseline characteristics may be significant.
This study is excluded in the after exclusion results of meta-analysis:
unadjusted results with significant baseline differences.
|
risk of death, 77.8% lower, RR 0.22, p = 0.01, treatment 3 of 60 (5.0%), control 9 of 40 (22.5%), NNT 5.7.
|
|
relative clinical score, 40.8% better, RR 0.59, p < 0.001, treatment 57, control 31.
|
|
relative CT score, 84.0% better, RR 0.16, p < 0.001, treatment 57, control 31.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Al-kuraishy et al., 1 Dec 2023, prospective, Iraq, peer-reviewed, 10 authors, study period March 2020 - June 2020.
Contact: engy.ali@pharm.tanta.edu.eg, dr_gaber_batiha@vetmed.dmu.edu.eg.
OBJECTIVE: Type 2 diabetes mellitus (T2DM) is regarded as a chief risk factor for(coronavirus disease 2019 (COVID-19) owing to dysregulation of the expression of angiotensin-converting enzyme 2 (ACE2) and chronic low-grade inflammatory disorders. Metformin, an insulin-sensitizing agent for managing T2DM, has pleiotropic anti-inflammatory and oxidant potentials, which may lessen the risk of diabetic complications. So, we aimed to reveal the potential role of metformin monotherapy in treating T2DM patients with COVID-19. PATIENTS AND METHODS: In this prospective cohort study, 60 hospitalized T2DM patients with COVID-19 on metformin plus standard anti-COVID-19 treatments compared to 40 hospitalized T2DM patients with COVID-19 on other diabetic pharmacotherapy like insulin and sulfonylurea, were recruited. Inflammatory and oxidative stress biomarkers and radiological and clinical outcomes were assessed at admission time and at the time of discharge. RESULTS: The results of this study illustrated that metformin treatment in T2DM patients with COVID-19 was more effective in reducing inflammatory and oxidative stress biomarkers with significant amelioration of radiological scores and clinical outcomes compared to T2DM patients with COVID-19 on another diabetic pharmacotherapy. CONCLUSIONS: Our findings highlighted that metformin efficiently managed T2DM patients with COVID-19 by reducing inflammatory and oxidative stress with mitigating effects on the radiological scores and clinical outcomes.
Conflict of Interest The authors declare that they have no conflict of interests.
Ethics Approval This study was approved scientific jury and the editorial board in the College of Medicine, Al-Mustansiriayiah University, Iraq, Baghdad (reference No. 34MTR on 20/2/2020).
Informed Consent Informed consent was obtained from all individual participants included in the study.
Authors' Contribution HMA and AAE performed the study, edited the main text, and approved the final edition of the manuscript. EEK, AA, MP, EE and GE-SB prepared the tables, wrote the main text, and approved the final edition of the manuscript. NA and RSH revised the manuscript. All authors approved the final edition of the manuscript.
References
Abdelaziz, Sonbol, Elbanna, El-Ekhnawy, Exposure to sublethal concentrations of benzalkonium chloride induces antimicrobial resistance and cellular changes in Klebsiellae pneumoniae clinical isolates, Microb Drug Resis
Abdelkader, Negm, Elekhnawy, Eliwa, Aldosari et al., Zinc Oxide Nanoparticles as Potential Delivery Carrier: Green Synthesis by Aspergillus niger Endophytic Fungus, Characterization, and In Vitro/In Vivo Antibacterial Activity, Pharm
Alherz, Negm, Elekhnawy, El-Masry, Haggag et al., Silver Nanoparticles Prepared Using Encephalartos laurentianus De Wild Leaf Extract Have Inhibitory Activity against Candida albicans Clinical Isolates, J Fungi
Almukainzi, El-Masry, Negm, Elekhnawy, Saleh et al., Co-delivery of gentiopicroside and thymoquinone using electrospun m-PEG/PVP nanofi-bers: In-vitro and In vivo studies for antibacterial wound dressing in diabetic rats, Intern J Pharm
Alomair, Al-Kuraishy, Ak, Gareeb, Waard et al., Is sitagliptin effective for SARS-CoV-2 infection: false or true prophecy?, Inflammopharmacol
Alotaibi, El-Masry, Elekhnawy, El-Kadem, Saleh et al., Aqueous core epigallocatechin gallate PLGA nanocapsules: Characterization, antibacterial activity against uropathogens, and in vivo reno-protective effect in cisplatin induced nephrotoxicity, Drug Deliv
Alotaibi, Negm, Elekhnawy, El-Masry, Elharty et al., Antibacterial activity of nano zinc oxide green-synthesised from Gardenia thailandica triveng. Leaves against Pseudomonas aeruginosa clinical isolates: in vitro and in vivo study, Art Cells Nanomed Biotechnol
Alwani, Yassin, Al-Zoubi, Aboumarzouk, Nettleship et al., Sex-based differences in severity and mortality in COVID-19, Rev Med Virol
Andrews, Mukhtar, Eze, Simoneau, Ross et al., Tropism of SARS-CoV-2 for human cortical astrocytes, Proceed Nation Acad Sci
Assoc, World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects, J Amer Collage Dentists
Attallah, El-Kadem, Negm, Elekhnawy, El-Masry et al., Promising Antiviral Activity of Agrimonia pilosa Phytochemicals against Severe Acute Respiratory Syndrome Coronavirus 2 Supported with In Vivo Mice Study, Pharm
Attallah, El-Sherbeni, El-Kadem, Elekhnawy, El-Masry et al., Elucidation of the metabolite profile of Yucca gigantea and assessment of its cytotoxic, antimicrobial, and anti-inflammatory activities, Mol
Attallah, Elekhnawy, Negm, Hussein, Mokhtar et al., In vivo and in vitro antimicrobial activity of biogenic silver nanoparticles against Staphylococcus aureus clinical isolates, Pharm
Attallah, Negm, Wa, Elekhnawy, Altwaijry et al., Antibacterial activity of Boswellia sacra Flueck. Oleoresin extract against Porphyromonas gingivalis periodontal pathogen, Antibiot
Attallah, Om, Elekhnawy, Hussein, Shaldam et al., Anti-biofilm and antibacterial activities of Cycas media R. Br secondary metabolites: In silico, in vitro, and in vivo approaches, Antibiot
Bao, Twigg, Shackel, Warner, Yue et al., Monocyte CD147 is induced by advanced glycation end products and high glucose concentration: possible role in diabetic complications, Amer J Phys Cell Phys
Batiha, Al-Kuraishy, Gareeb, Elekhnawy, SIRT1 pathway in Parkinson's disease: a faraway snapshot but so close, Inflammopharmacol
Batiha, Gareeb, Elekhnawy, Hm, Potential role of lipoxin in the management of COVID-19: a narrative review, Inflammopharmacol
Bramante, Ingraham, Murray, Marmor, Observational study of metformin and risk of mortality in patients hospitalized with Covid-19, MedRxiv
Bramante, Ingraham, Murray, Metformin and risk of mortality in patients hospitalised with COVID-19: a retrospective cohort analysis, Lancet Health Long
Chakraborty, Chowdhury, Bhattacharyya, Effect of metformin on oxidative stress, nitrosative stress and inflammatory biomarkers in type 2 diabetes patients, Diabetes Res Clin Pract
Coll, Chen, Taskar, Rimmington, Patel et al., GDF15 mediates the effects of metformin on body weight and energy balance, Nature
Cory, Emmons, Yarbro, Davis, Pence, Metformin suppresses monocyte immunometabolic activation by SARS-CoV-2 spike protein subunit 1, Front Immunol
Cuthbertson, Patterson, Harte, Bell, Investigation of the effect of oral metformin on dipeptidylpeptidase-4 (DPP-4) activity in Type 2 diabetes 1, Diabet Med
Dehkordi, Abbaszadeh, Mir, Hasanvand, Metformin and its anti-inflammatory and anti-oxidative effects; new concepts, J Renal Injury Preven
Du, Wang, Chen, The potential effects of DPP-4 inhibitors on cardiovascular system in COVID-19 patients, J Cell Mol Med
Elekhnawy, Negm, The potential application of probiotics for the prevention and treatment of COVID-19, Egypt J Med Hum Genet
Elekhnawy, Sonbol, Elbanna, Abdelaziz, Evaluation of the impact of adaptation of Klebsiella pneumoniae clinical isolates to benzalkonium chloride on biofilm formation, Egyp J Med Hum Gen
Floch, Chiche, Marchiq, Naiken, Ilc et al., Growth inhibition of glycolytic tumors by targeting basigin/lactate-H+ symporters (MCTs): metformin sensitizes MCT inhibition, Cancer Res
Flory, Lipska, Metformin in 2019, JAMA
Fontaine, Metformin and respiratory chain complex I: the last piece of the puzzle?, Biochem J
Fontaine, Metformin-induced mitochondrial complex I inhibition: facts, uncertainties, and consequences, Front Endocrinol
Gomez, Du-Fay-De-Lavallaz, Fugar, Sarau, Simmons et al., Sex differences in COVID-19 hospitalization and mortality, J Wom Health
He, Metformin and systemic metabolism, Trends Pharmacol Sci
Hm, Gareeb, Alblihed, Guerreiro, Cruz-Martins et al., COVID-19 in relation to hyperglycemia and diabetes mellitus, Front Cardio Med
Hm, Gareeb, Albogami, Jean-Marc, Nadwa et al., Potential therapeutic benefits of metformin alone and in combination with sitagliptin in the management of type 2 diabetes patients with COVID-19, Pharm
Hm, Gareeb, Elekhnawy, Batiha, Dipyridamole and adenosinergic pathway in Covid-19: a juice or holy grail, Egyp J Med Hum Gen
Hm, Gareeb, Elekhnawy, Batiha, Nitazoxanide and COVID-19: a review, Mol Biolog Rep
Hm, Gareeb, Ha, Al-Harcan, Alexiou et al., Neutrophil Extracellular Traps (NETs) and Covid-19: A new frontiers for therapeutic modality, Int Immunopharmacol
Hm, Gareeb, Kaushik, Kujawska, Batiha, Hemolytic anemia in COVID-19, Ann Hematol
Hm, Om, Elekhnawy, Gareeb, Alorabi et al., Traditional herbs against COVID-19: back to old weapons to combat the new pandemic, Europ J Med Res
Kamyshnyi, Matskevych, Lenchuk, Strilbytska, Storey et al., Metformin to decrease COVID-19 severity and mortality: Molecular mechanisms and therapeutic potential, Biomed Pharmacother
Khudhair, Gareeb, Hm, El-Kadem, Elekhnawy et al., Combination of vitamin C and curcumin safeguards against methotrexate-induced acute liver injury in mice by synergistic antioxidant effects, Front Med
Koepsell, Role of organic cation transporters in drug-drug interaction, Expert Opin Drug Metab Toxicol
Kotagale, Rahangdale, Borkar, Singh, Ikhar et al., Possible involvement of agmatine in neuropharmacological actions of metformin in diabetic mice, Eur J Pharmacol
Kočar, Režen, Rozman, Cholesterol, lipoproteins, and COVID-19: Basic concepts and clinical applications, Biochimica et Biophysica Acta (BBA). Mol Cell Biol Lip
Lamoia, Shulman, Cellular and molecular mechanisms of metformin action, Endocr Rev
Liu, Mei, Chen, Qin, Li et al., Protective effect of agmatine against hyperoxia-induced acute lung injury via regulating lncRNA gadd7, Biochem Biophys Res Commun
Lukito, Pranata, Henrina, Lim, Lawrensia et al., The effect of metformin consumption on mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis, Diabetes Metab Syndr Clin Res Rev
Lv, Guo, Metformin and its benefits for various diseases, Front Endocrinol
Markowicz-Piasecka, Huttunen, Mateusiak, Mikiciuk-Olasik, Sikora, Sulfenamide and sulfonamide derivatives of metformin can exert anticoagulant and profibrinolytic properties, Chem Biol Interact
Masana, Correig, Ibarretxe, Anoro, Arroyo et al., Low HDL and high triglycerides predict COVID-19 severity, Sci Rep
Ms, Hm, Gareeb, Mamoori, Metabolic profile and prolactin serum levels in men with type 2 diabetes mellitus: Old-new rubric, Inter J Crit Illness Injury Sci
Nadwa, Al-Kuraishy, Gareeb, Elekhnawy, Albogami et al., Cholinergic dysfunction in COVID-19: frantic search and hoping for the best, Naunyn-Schmiedeberg's Arch Pharmacol
Naji, Shams, Sami, Al-Harchan, Hm et al., Oxidative stress injury and glucolipotoxicity in type 2 diabetes mellitus: The potential role of metformin and sitagliptin, BBRJ
Naji, Shams, Sami, Al-Kuraishy, Gareeb, Erectile dysfunction and type 2 diabetes mellitus: a new twist, ter J Nut Pharmacol Neurol Dis
Negm, El-Aasr, Kamer, Elekhnawy, Investigation of the Antibacterial Activity and Efflux Pump Inhibitory Effect of Cycas thouarsii R. Br. Extract against Klebsiella pneumoniae Clinical Isolates, Pharm
Ojeda-Fernández, Foresta, Macaluso, Colacioppo, Tettamanti et al., Metformin use is associated with a decrease in the risk of hospitalization and mortality in COVID-19 patients with diabetes: A population-based study in Lombardy, Diab Obes Met
Onohuean, Al-Kuraishy, Gareeb, Qusti, Alshammari et al., Covid-19 and development of heart failure: mystery and truth, Naunyn-Schmiedebergs Arch Pharmacol
Parthasarathy, Tandel, Siddiqui, Harshan, Metformin suppresses SARS-CoV-2 in cell culture, Virus Res
Paul, Hossain, Mahboob, Nissapatorn, Wilairatana et al., Does oxidative stress management help alleviation of COVID-19 symptoms in patients experiencing diabete, Nutrients
Pivonello, Auriemma, Pivonello, Isidori, Corona et al., Sex disparities in COVID-19 severity and outcome: are men weaker or women stronger?, Neuroendocrinol
Pollizzi, Patel, Sun, Oh, Waickman et al., mTORC1 and mTORC2 selectively regulate CD8+ T cell differentiation, J Clin invest
Radzikowska, Ding, Tan, Zhakparov, Peng et al., Distribution of ACE2, CD147, CD26, and other SARS-CoV-2 associated molecules in tissues and immune cells in health and in asthma, COPD, obesity, hypertension, and COVID-19 risk factors, Allergy
Rasheed, Hm, Gareeb, Hussien, Ms, Effects of diabetic pharmacotherapy on prolactin hormone in patients with type 2 diabetes mellitus: Bane or Boon, J Adv Pharm Technol Res
Rochette, Zeller, Cottin, Vergely, GDF15: an emerging modulator of immunity and a strategy in COVID-19 in association with iron metabolism, Trends Endocrinol Metab
Salvatore, Pafundi, Morgillo, Liello, Galiero et al., Metformin: An old drug against old age and associated morbidities, Diabetes Res Clin Pract
Samuel, Varghese, Büsselberg, Therapeutic potential of metformin in COVID-19: reasoning for its protective role, Trends Microbiol
Sanoudou, Hill, Belanger, Arao, Mantzoros, Editorial: Obesity, metabolic phenotypes and COVID-19, Met Clin Exp
Shrestha, Foster, Rawlinson, Tedla, Bull, Evolution of the SARS-CoV-2 omicron variants BA. 1 to BA. 5: Implications for immune escape and transmission, Rev Med Virol
Singh, Gupta, Ghosh, Misra, Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations. Diabetes & Metabolic Syndrome, Clin Res Rev
Singh, Gupta, Misra, Comorbidities in COVID-19: Outcomes in hypertensive cohort and controversies with renin angiotensin system blockers, Diabetes Metab Syndr
Sonbol, El-Banna, El-Aziz, El-Ekhnawy, Impact of triclosan adaptation on membrane properties, efflux and antimicrobial resistance of Escherichia coli clinical isolates, J App Microbiol
Tsaknis, Siempos, Kopterides, Maniatis, Magkou et al., Metformin attenuates ventilator-induced lung injury, Crit Care
Usman, Bliden, Cho, Walia, Jerjian et al., Metformin use in patients hospitalized with COVID-19: lower inflammation, oxidative stress, and thrombotic risk markers and better clinical outcomes, J Thromb Thrombolysis
Vial, Detaille, Guigas, Role of mitochondria in the mechanism (s) of action of metformin, Front Endocrinol
Viollet, Guigas, Garcia, Leclerc, Foretz et al., Cellular and molecular mechanisms of metformin: an overview, Clin Sci
Xin, Wei, Ji, Zheng, Gu et al., Metformin uniquely prevents thrombosis by inhibiting platelet activation and mtDNA release, Sci Rep
Yang, Sun, Zhang, Zhang, The effect of metformin on mortality and severity in COVID-19 patients with diabetes mellitus, Diabetes Res Clin Pract
Yang, Zheng, Gou, Pu, Chen et al., Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis, Int J Infect Dis
Zangiabadian, Nejadghaderi, Zahmatkesh, Hajikhani, Mirsaeidi et al., The efficacy and potential mechanisms of metformin in the treatment of COVID-19 in the diabetics: a systematic review, Front Endocrinol
Zhang, Dong, Martin, He, Gongol et al., AMP-activated protein kinase phosphorylation of angiotensin-converting enzyme 2 in endothelium mitigates pulmonary hypertension, Am J Respir Crit Care Med
DOI record:
{
"DOI": "10.26355/eurrev_202312_34583",
"ISSN": "1128-3602, 2284-0729",
"URL": "https://doi.org/10.26355/eurrev_202312_34583",
"abstract": "OBJECTIVE: Type 2 diabetes mellitus (T2DM) is regarded as a chief risk factor for(coronavirus disease 2019 (COVID-19) owing to dysregulation of the expression of angiotensin-converting enzyme 2 (ACE2) and chronic low-grade inflammatory disorders. Metformin, an insulin-sensitizing agent for managing T2DM, has pleiotropic anti-inflammatory and oxidant potentials, which may lessen the risk of diabetic complications. So, we aimed to reveal the potential role of metformin monotherapy in treating T2DM patients with COVID-19. PATIENTS AND METHODS: In this prospective cohort study, 60 hospitalized T2DM patients with COVID-19 on metformin plus standard anti-COVID-19 treatments compared to 40 hospitalized T2DM patients with COVID-19 on other diabetic pharmacotherapy like insulin and sulfonylurea, were recruited. Inflammatory and oxidative stress biomarkers and radiological and clinical outcomes were assessed at admission time and at the time of discharge. RESULTS: The results of this study illustrated that metformin treatment in T2DM patients with COVID-19 was more effective in reducing inflammatory and oxidative stress biomarkers with significant amelioration of radiological scores and clinical outcomes compared to T2DM patients with COVID-19 on another diabetic pharmacotherapy. CONCLUSIONS: Our findings highlighted that metformin efficiently managed T2DM patients with COVID-19 by reducing inflammatory and oxidative stress with mitigating effects on the radiological scores and clinical outcomes.",
"author": [
{
"family": "Al-kuraishy",
"given": "H.M."
},
{
"family": "Al-Gareeb",
"given": "A.I."
},
{
"family": "El Kholy",
"given": "A.A."
},
{
"family": "El-Khateeb",
"given": "E."
},
{
"family": "Alexiou",
"given": "A."
},
{
"family": "Papadakis",
"given": "M."
},
{
"family": "Elekhnawy",
"given": "E."
},
{
"family": "Alsubaie",
"given": "N."
},
{
"family": "Hamad",
"given": "R.S."
},
{
"family": "Batiha",
"given": "G.E."
}
],
"container-title": "European Review for Medical and Pharmacological Sciences",
"issue": "23",
"issued": {
"date-parts": [
[
2023,
12
]
]
},
"language": "eng",
"medium": "JB",
"page": "11445-11456",
"page-first": "11445",
"publisher": "Verduci Editore s.r.l.",
"publisher-place": "IT",
"title": "The potential therapeutic effect of metformin in type 2 diabetic patients with severe COVID-19",
"type": "article-journal",
"volume": "27"
}
