Causal Inference and COVID-19 Nursing Home Patients: Identifying Factors That Reduced Mortality Risk
et al., medRxiv, doi:10.1101/2021.11.18.21266489, Nov 2021
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective causal inference analysis of 4,091 COVID+ long-term care high risk patients in the USA, showing lower mortality with vitamin D, without statistical significance.
This is the 59th of 135 COVID-19 controlled studies for vitamin D, which collectively show efficacy with p<0.0000000001.
40 studies are RCTs, which show efficacy with p=0.0000001.
Standard of Care (SOC) for COVID-19 in the study country,
the USA, is very poor with very low average efficacy for approved treatments1.
Only expensive, high-profit treatments were approved for early treatment. Low-cost treatments were excluded, reducing the probability of early treatment due to access and cost barriers, and eliminating complementary and synergistic benefits seen with many low-cost treatments.
|
risk of death, 10.5% lower, RR 0.90, p = 0.28.
|
| Effect extraction follows pre-specified rules prioritizing more serious outcomes. Submit updates |
Ahmed et al., 21 Nov 2021, retrospective, USA, preprint, 5 authors, dosage not specified.
Causal Inference and COVID-19 Nursing Home Patients: Identifying Factors That Reduced Mortality Risk
doi:10.1101/2021.11.18.21266489
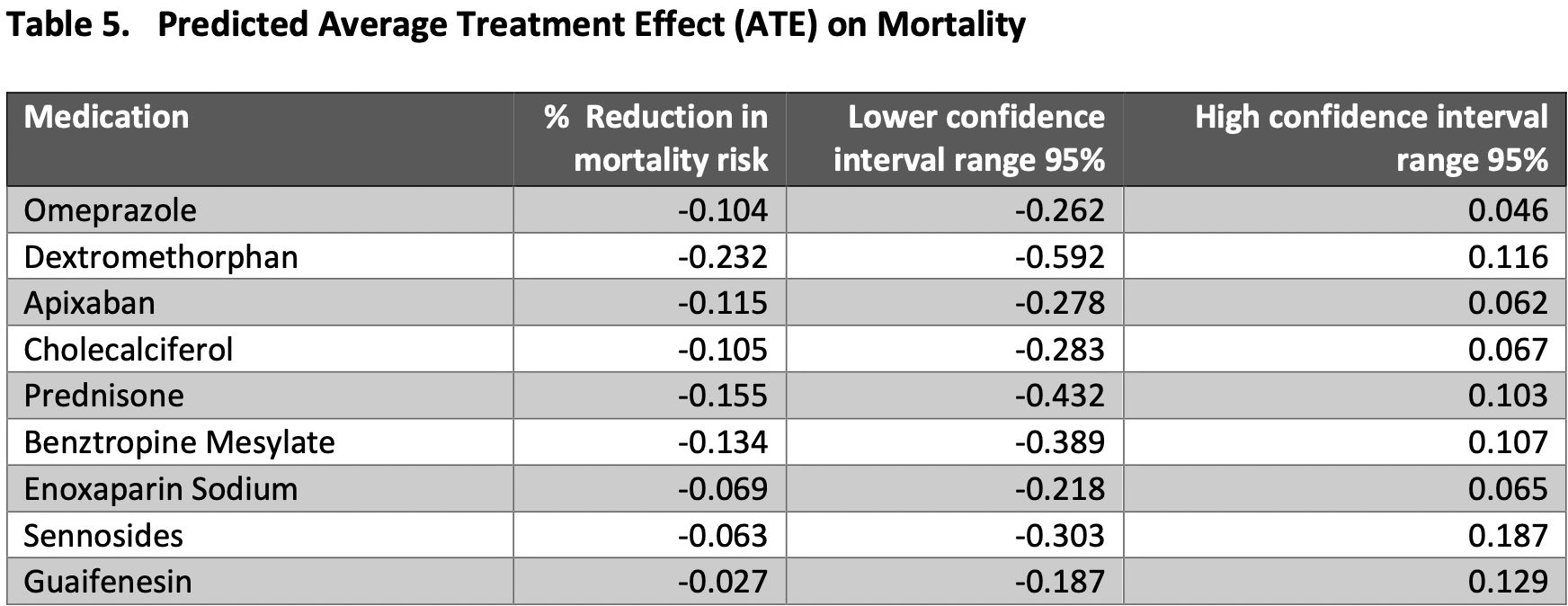
Less than 1% of the US population lives in long-term care facilities, yet this subset of the population accounts for 22% of total COVID-19 related deaths. 1 Because of a lack of experimental evidence to treat COVID-19, analysis of real-world data to identify causal relationships between treatments/policies to mortality and morbidity among high-risk individuals is critical. We applied causal inference (CI) analysis to longitudinal patient-level health data of 4,091 long-term care high-risk patients with COVID-19 to determine if any actions or therapies delivered from January to August of 2020 reduced COVID-19 patient mortality rates during this period. Causal inference findings determined that certain supportive care interventions caused reduced mortality rates for nursing home residents regardless of severity of disease (as measured by oxygen saturation level, presence of pneumonia and organ failure), comorbidities or social determinants of health such as race, age, and weight. 2 While we do not address the biological mechanisms associated with specific medical interventions and their impact on mortality, this analysis suggests methods to validate and optimize treatment protocols using domain knowledge and causal inference analysis of real-world data across patient populations and care settings.
References
Arabi, Gordon, Derde, Lopinavir-ritonavir and hydroxychloroquine for critically ill patients with COVID-19: REMAP-CAP randomized controlled trial, Intensive Care Med, doi:10.1007/s00134-021-06448-5
Bagchi, Mak, Li, Rates of COVID-19 Among Residents and Staff Members in Nursing Homes -United States, May 25, MMWR Morb Mortal Wkly Rep, doi:10.15585/mmwr.mm7002e2externalicon
Balzer, Petersen, Van Der Laan, Search Collaboration, Targeted estimation and inference for the sample average treatment effect in trials with and without pair-matching, Stat Med, doi:10.1002/sim.6965
Bareinboim, Pearl, Causal inference and the data-fusion problem, Proc Natl Acad Sci U S A, doi:10.1073/pnas.1510507113
Hager, Tsiatis, Davidian, Optimal two-stage dynamic treatment regimes from a classification perspective with censored survival data, Biometrics, doi:10.1111/biom.12894
Kosar, White, Feifer, COVID-19 Mortality Rates Among Nursing Home Residents Declined from March to November 2020, Health Aff (Millwood), doi:10.1377/hlthaff.2020.02191
Mackenzie, Race, COVID Mortality, and Simpson's Paradox
Mohan, Pearl, Graphical Models for Processing Missing Data, Journal of the American Statistical Association, doi:10.1080/01621459.2021.1874961
Oprescu, Syrgkanis, Wu, Orthogonal Random Forest for Causal Inference
Pearl, On the Testability of Causal Models with Latent and Instrumental Variables
Pearl, The seven tools of causal inference, with reflections on machine learning, Communications of the ACM, doi:10.1145/3241036
Pedregosa, Scikit-learn: Machine Learning in Python, JMLR
Prosperi, Guo, Sperrin, Causal inference and counterfactual prediction in machine learning for actionable healthcare, Nat Mach Intell, doi:10.1038/s42256-020-0197-y
Prosperi, Guo, Sperrin, Causal inference and counterfactual prediction in machine learning for actionable healthcare, Nat Mach Intell, doi:10.1038/s42256-020-0197-y
Tarazi, Finegold, Sheingold, Samson, Zuckerman et al., COVID-19-Related Deaths And Excess Deaths Among Medicare Fee-For-Service Beneficiaries, Health Aff (Millwood), doi:10.1377/hlthaff.2020.02521
DOI record:
{
"DOI": "10.1101/2021.11.18.21266489",
"URL": "http://dx.doi.org/10.1101/2021.11.18.21266489",
"abstract": "<jats:title>Abstract</jats:title><jats:p>Less than 1% of the US population lives in long-term care facilities, yet this subset of the population accounts for 22% of total COVID-19 related deaths.<jats:sup>1</jats:sup> Because of a lack of experimental evidence to treat COVID-19, analysis of real-world data to identify causal relationships between treatments/policies to mortality and morbidity among high-risk individuals is critical. We applied causal inference (CI) analysis to longitudinal patient-level health data of 4,091 long-term care high-risk patients with COVID-19 to determine if any actions or therapies delivered from January to August of 2020 reduced COVID-19 patient mortality rates during this period.</jats:p><jats:p>Causal inference findings determined that certain supportive care interventions caused reduced mortality rates for nursing home residents regardless of severity of disease (as measured by oxygen saturation level, presence of pneumonia and organ failure), comorbidities or social determinants of health such as race, age, and weight.<jats:sup>2</jats:sup> While we do not address the biological mechanisms associated with specific medical interventions and their impact on mortality, this analysis suggests methods to validate and optimize treatment protocols using domain knowledge and causal inference analysis of real-world data across patient populations and care settings.</jats:p>",
"accepted": {
"date-parts": [
[
2021,
11,
21
]
]
},
"author": [
{
"affiliation": [],
"family": "Ahmed",
"given": "Amina",
"sequence": "first"
},
{
"affiliation": [],
"family": "Goldberg",
"given": "Robert",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Swiader",
"given": "Joseph",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Wintrob",
"given": "Zachary A.P.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Yilmaz",
"given": "Margaret",
"sequence": "additional"
}
],
"container-title": [],
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2021,
11,
21
]
],
"date-time": "2021-11-21T19:25:17Z",
"timestamp": 1637522717000
},
"deposited": {
"date-parts": [
[
2021,
11,
24
]
],
"date-time": "2021-11-24T06:35:12Z",
"timestamp": 1637735712000
},
"group-title": "Health Systems and Quality Improvement",
"indexed": {
"date-parts": [
[
2021,
12,
18
]
],
"date-time": "2021-12-18T16:04:09Z",
"timestamp": 1639843449658
},
"institution": [
{
"name": "medRxiv"
}
],
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2021,
11,
21
]
]
},
"link": [
{
"URL": "https://syndication.highwire.org/content/doi/10.1101/2021.11.18.21266489",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "246",
"original-title": [],
"posted": {
"date-parts": [
[
2021,
11,
21
]
]
},
"prefix": "10.1101",
"published": {
"date-parts": [
[
2021,
11,
21
]
]
},
"publisher": "Cold Spring Harbor Laboratory",
"reference-count": 0,
"references-count": 0,
"relation": {},
"score": 1,
"short-container-title": [],
"short-title": [],
"source": "Crossref",
"subtitle": [],
"subtype": "preprint",
"title": [
"Causal Inference and COVID-19 Nursing Home Patients: Identifying Factors That Reduced Mortality Risk"
],
"type": "posted-content"
}
