Estimates of Incidence and Predictors of Fatiguing Illness after SARS-CoV-2 Infection
et al., Emerging Infectious Diseases, doi:10.3201/eid3003.231194, Mar 2024
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
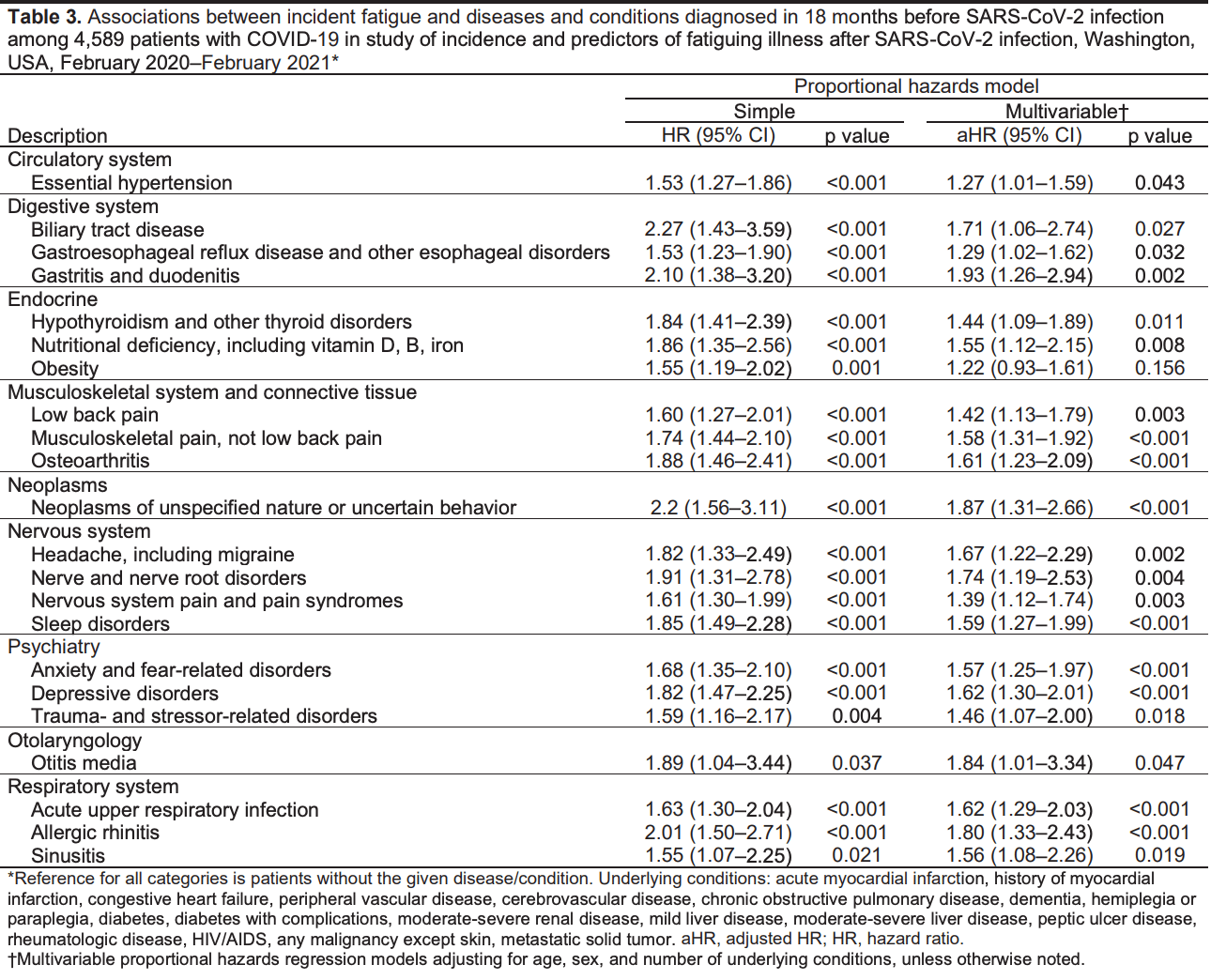
Retrospective 4,589 COVID-19 patients and 9,022 matched controls showing that COVID-19 patients had a significantly higher risk of developing fatigue and chronic fatigue. Among COVID-19 patients, nutritional deficiency (including vitamin D, B, and iron) was associated with higher risk of fatiguing illness.
Vu et al., 1 Mar 2024, retrospective, USA, peer-reviewed, mean age 49.5, 8 authors.
Estimates of Incidence and Predictors of Fatiguing Illness after SARS-CoV-2 Infection
Emerging Infectious Diseases, doi:10.3201/eid3003.231194
A ccording to the Household Pulse Survey con- ducted by the US Centers for Disease Control and Prevention in January 2023, up to 15% of all US adults had experienced >1 symptoms of post-COVID-19 conditions (PCC), also known as long COVID or postacute sequelae of SARS-CoV-2 infection (PASC) (1). Among persons with PCC, fatigue is frequently reported in both hospitalized and nonhospitalized patients (2,3). A recent prospective cohort study reported 85% of patients who met its PASC definition had fatigue (4). A substantial percentage of patients with fatigue remain ill for many months with an illness similar to myalgic encephalomyelitis/ chronic fatigue syndrome (ME/CFS) ( 5 ), an unexplained syndrome sometimes seen after infections that is characterized by functional limitations that impair patients' ability to maintain daily activities and is associated with profound fatigue (6). The burden, distribution, and trend of PCC can theoretically be measured by using prevalence and incidence. The prevalence of PCC is a useful measure of overall disease burden at a specific time but is dependent on recovery, deaths, and incidence. The incidence of PCC measures the rate of new cases over a certain period and can be valuable for informing public health actions to reduce new illnesses. Numerous studies have estimated PCC prevalence, but very few have attempted to estimate PCC incidence because the incidence estimate requires information on timing of incident event and a well-defined population at risk that does not include prevalent cases (7). Both requirements are challenging in the context of PCC because they consist of a range of conditions and symptoms, most of which are not specific to PCC. To date, no diagnostic biomarkers are available, and recognition of PCC requires integrating medical history and clinical findings. Recent studies also emphasize the importance of an equivalent, concurrent, non-COVID-19 comparison group so that the effects of COVID-19 will not be overestimated (8). Given the central role of fatigue in PCC and the lack of data on incidence of fatigue among patients who have had COVID-19, we conducted a study of incident fatigue diagnoses among patients with and without COVID-19. Our objectives were to estimate the incidence rates of fatigue and chronic fatigue; quantify the additional incident fatigue caused by COVID-19; assess factors associated with incident fatigue; and describe deaths and hospitalizations among patients with incident fatigue after SARS-CoV-2 infection.
S crapie is a fatal neurodegenerative disease of sheep and goats that was the first of a group of spongiform encephalopathies to be reported (1732 in England) and the first whose transmissibility was demonstrated by Cuille and Chelle in 1936. The name resulted because most affected sheep develop pruritis and compulsively scratch their hides against fixed objects. Like other transmissible spongiform encephalopathies, scrapie is associated with an alteration in conformation of a normal neural cell glycoprotein, the prion protein. The scrapie agent was first described as a prion (and the term coined) by Stanley Prusiner in 1982, work for which he received the Nobel Prize in 1997.
References
Bateman, Bested, Bonilla, Chheda, Chu et al., Myalgic Encephalomyelitis/chronic fatigue syndrome: essentials of diagnosis and management, Mayo Clin Proc, doi:10.1016/j.mayocp.2021.07.004
Brown, Bradley, 1755 and all that: a historical primer of transmissible spongiform encephalopathy, BMJ
Carfì, Bernabei, Landi, Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19, JAMA, doi:10.1001/jama.2020.12603
Castro, Gunning, Mccoy, Perlis, Mood disorders and outcomes of COVID-19 hospitalizations, Am J Psychiatry
Charlson, Pompei, Ales, Mackenzie, A new method of classifying prognostic comorbidity in longitudinal studies: development and validation, J Chronic Dis, doi:10.1016/0021-9681(87)90171-8
Choutka, Jansari, Hornig, Iwasaki, Unexplained post-acute infection syndromes, Nat Med, doi:10.1038/s41591-022-01810-6
Cuillé, Chelle, The so-called "trembling" disease of sheep: is it inoculable?, Comptes Rendus de l'Académie Sciences
Daugherty, Guo, Heath, Dasmariñas, Jubilo et al., Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study, BMJ, doi:10.1136/bmj.n1098
Goklemez, Saligan, Pirsl, Holtzman, Ostojic et al., Clinical characterization and cytokine profile of fatigue in hematologic malignancy patients with chronic graft-versus-host disease, Bone Marrow Transplant, doi:10.1038/s41409-021-01419-2
Gottlieb, Wang, Yu, Spatz, Montoy et al., Innovative Support for Patients with SARS-CoV-2 Infections Registry (INSPIRE) Group. Severe fatigue and persistent symptoms at 3 months following severe acute respiratory syndrome coronavirus 2 infections during the pre-Delta, Delta, and Omicron time periods: a multicenter prospective cohort study, Clin Infect Dis, doi:10.1093/cid/ciad045
Horberg, Watson, Bhatia, Jefferson, Certa et al., Post-acute sequelae of SARS-CoV-2 with clinical condition definitions and comparison in a matched cohort, Nat Commun, doi:10.1038/s41467-022-33573-6
Laplanche, Hunter, Shinagawa, Williams, Scrapie, chronic wasting disease, and transmissible mink encephalopathy
Lin, Wei, The robust inference for the Cox proportional hazards model, J Am Stat Assoc, doi:10.1080/01621459.1989.10478874
O'mahoney, Routen, Gillies, Ekezie, Welford et al., The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis, EClinicalMedicine, doi:10.1016/j.eclinm.2022.101762
Prusiner, Novel proteinaceous infectious particles cause scrapie, Science
Quan, Li, Couris, Fushimi, Graham et al., Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries, Am J Epidemiol, doi:10.1093/aje/kwq433
Quan, Vu, vaq2@cdc, Emerging Infectious Diseases •
Roessler, Tesch, Batram, Jacob, Loser et al., Post-COVID-19-associated morbidity in children, adolescents, and adults: a matched cohort study including more than 157,000 individuals with COVID-19 in Germany, PLoS Med, doi:10.1371/journal.pmed.1004122
Rosenbaum, Db, The central role of the propensity score in observational studies for causal effects, Biometrika, doi:10.1093/biomet/70.1.41
Taquet, Dercon, Luciano, Geddes, Husain et al., Incidence, co-occurrence, and evolution of long-COVID features: a 6-month retrospective cohort study of 273,618 survivors of COVID-19, PLoS Med, doi:10.1371/journal.pmed.1003773
Thaweethai, Jolley, Karlson, Levitan, Levy et al., RECOVER Consortium. Development of a definition of postacute sequelae of SARS-CoV-2 infection, JAMA, doi:10.1001/jama.2023.8823
Thomas, Motivala, Olmstead, Irwin, Sleep depth and fatigue: role of cellular inflammatory activation, Brain Behav Immun, doi:10.1016/j.bbi.2010.07.245
Wisk, Gottlieb, Spatz, Yu, Wang et al., Association of initial SARS-CoV-2 test positivity with patient-reported well-being 3 months after a symptomatic illness, JAMA Netw Open, doi:10.1001/jamanetworkopen.2022.44486
Zhang, Kim, Lonjon, Zhu, Balance diagnostics after propensity score matching, Ann Transl Med, doi:10.21037/atm.2018.12.10
DOI record:
{
"DOI": "10.3201/eid3003.231194",
"ISSN": [
"1080-6040",
"1080-6059"
],
"URL": "http://dx.doi.org/10.3201/eid3003.231194",
"author": [
{
"affiliation": [],
"family": "Vu",
"given": "Quan M.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Fitzpatrick",
"given": "Annette L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cope",
"given": "Jennifer R.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Bertolli",
"given": "Jeanne",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Sotoodehnia",
"given": "Nona",
"sequence": "additional"
},
{
"affiliation": [],
"family": "West",
"given": "T. Eoin",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Gentile",
"given": "Nikki",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Unger",
"given": "Elizabeth R.",
"sequence": "additional"
}
],
"container-title": "Emerging Infectious Diseases",
"container-title-short": "Emerg. Infect. Dis.",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2024,
2,
23
]
],
"date-time": "2024-02-23T17:05:01Z",
"timestamp": 1708707901000
},
"deposited": {
"date-parts": [
[
2024,
2,
23
]
],
"date-time": "2024-02-23T17:05:05Z",
"timestamp": 1708707905000
},
"indexed": {
"date-parts": [
[
2024,
2,
24
]
],
"date-time": "2024-02-24T00:36:16Z",
"timestamp": 1708734976011
},
"is-referenced-by-count": 0,
"issue": "3",
"issued": {
"date-parts": [
[
2024,
3
]
]
},
"journal-issue": {
"issue": "3",
"published-print": {
"date-parts": [
[
2024,
3
]
]
}
},
"member": "1822",
"original-title": [],
"prefix": "10.3201",
"published": {
"date-parts": [
[
2024,
3
]
]
},
"published-print": {
"date-parts": [
[
2024,
3
]
]
},
"publisher": "Centers for Disease Control and Prevention (CDC)",
"reference": [
{
"key": "key-10.3201/eid3003.231194-202402141031-R1",
"unstructured": "Centers for Disease Control and Prevention. Long COVID—household pulse survey [cited 2023 Feb 6]. https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm"
},
{
"DOI": "10.1001/jama.2020.12603",
"article-title": "Persistent symptoms in patients after acute COVID-19.",
"author": "Carfì",
"doi-asserted-by": "publisher",
"first-page": "603",
"journal-title": "JAMA",
"key": "key-10.3201/eid3003.231194-202402141031-R2",
"volume": "324",
"year": "2020"
},
{
"DOI": "10.1016/j.eclinm.2022.101762",
"article-title": "The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis.",
"author": "O’Mahoney",
"doi-asserted-by": "publisher",
"first-page": "101762",
"journal-title": "EClinicalMedicine",
"key": "key-10.3201/eid3003.231194-202402141031-R3",
"volume": "55",
"year": "2022"
},
{
"DOI": "10.1001/jama.2023.8823",
"article-title": "RECOVER Consortium. Development of a definition of postacute sequelae of SARS-CoV-2 infection.",
"author": "Thaweethai",
"doi-asserted-by": "publisher",
"first-page": "1934",
"journal-title": "JAMA",
"key": "key-10.3201/eid3003.231194-202402141031-R4",
"volume": "329",
"year": "2023"
},
{
"DOI": "10.1016/j.mayocp.2021.07.004",
"article-title": "Myalgic Encephalomyelitis/chronic fatigue syndrome: essentials of diagnosis and management.",
"author": "Bateman",
"doi-asserted-by": "publisher",
"first-page": "2861",
"journal-title": "Mayo Clin Proc",
"key": "key-10.3201/eid3003.231194-202402141031-R5",
"volume": "96",
"year": "2021"
},
{
"DOI": "10.1038/s41591-022-01810-6",
"article-title": "Unexplained post-acute infection syndromes.",
"author": "Choutka",
"doi-asserted-by": "publisher",
"first-page": "911",
"journal-title": "Nat Med",
"key": "key-10.3201/eid3003.231194-202402141031-R6",
"volume": "28",
"year": "2022"
},
{
"DOI": "10.1038/s41467-022-33573-6",
"article-title": "Post-acute sequelae of SARS-CoV-2 with clinical condition definitions and comparison in a matched cohort.",
"author": "Horberg",
"doi-asserted-by": "publisher",
"first-page": "5822",
"journal-title": "Nat Commun",
"key": "key-10.3201/eid3003.231194-202402141031-R7",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1001/jamanetworkopen.2022.44486",
"article-title": "INSPIRE Group. Association of initial SARS-CoV-2 test positivity with patient-reported well-being 3 months after a symptomatic illness.",
"author": "Wisk",
"doi-asserted-by": "publisher",
"first-page": "e2244486",
"journal-title": "JAMA Netw Open",
"key": "key-10.3201/eid3003.231194-202402141031-R8",
"volume": "5",
"year": "2022"
},
{
"key": "key-10.3201/eid3003.231194-202402141031-R9",
"unstructured": "Centers for Disease Control and Prevention. ICD-10-CM official coding and reporting guidelines: April 1, 2020 through September 30, 2020 [cited 2023 Aug 25]. https://www.cdc.gov/nchs/data/icd/covid-19-guidelines-final.pdf"
},
{
"key": "key-10.3201/eid3003.231194-202402141031-R10",
"unstructured": "Centers for Disease Control and Prevention. Co-occurrence of other respiratory illnesses for hospital confirmed COVID-19 encounters by week from selected hospitals [cited 2023 Mar 10]. https://www.cdc.gov/nchs/covid19/nhcs/other-respiratory-illnesses.htm"
},
{
"DOI": "10.1093/biomet/70.1.41",
"article-title": "The central role of the propensity score in observational studies for causal effects.",
"author": "Rosenbaum",
"doi-asserted-by": "publisher",
"first-page": "41",
"journal-title": "Biometrika",
"key": "key-10.3201/eid3003.231194-202402141031-R11",
"volume": "70",
"year": "1983"
},
{
"DOI": "10.1016/0021-9681(87)90171-8",
"article-title": "A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.",
"author": "Charlson",
"doi-asserted-by": "publisher",
"first-page": "373",
"journal-title": "J Chronic Dis",
"key": "key-10.3201/eid3003.231194-202402141031-R12",
"volume": "40",
"year": "1987"
},
{
"DOI": "10.21037/atm.2018.12.10",
"article-title": "Balance diagnostics after propensity score matching.",
"author": "Zhang",
"doi-asserted-by": "publisher",
"first-page": "16",
"journal-title": "Ann Transl Med",
"key": "key-10.3201/eid3003.231194-202402141031-R13",
"volume": "7",
"year": "2019"
},
{
"DOI": "10.1080/01621459.1989.10478874",
"article-title": "The robust inference for the Cox proportional hazards model.",
"author": "Lin",
"doi-asserted-by": "publisher",
"first-page": "1074",
"journal-title": "J Am Stat Assoc",
"key": "key-10.3201/eid3003.231194-202402141031-R14",
"volume": "84",
"year": "1989"
},
{
"key": "key-10.3201/eid3003.231194-202402141031-R15",
"unstructured": "Agency for Healthcare Research and Quality. Clinical Classifications Software Refined (CCSR) [cited 2023 Jan 19]. https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp"
},
{
"DOI": "10.1093/aje/kwq433",
"article-title": "Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries.",
"author": "Quan",
"doi-asserted-by": "publisher",
"first-page": "676",
"journal-title": "Am J Epidemiol",
"key": "key-10.3201/eid3003.231194-202402141031-R16",
"volume": "173",
"year": "2011"
},
{
"DOI": "10.1371/journal.pmed.1003773",
"article-title": "Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19.",
"author": "Taquet",
"doi-asserted-by": "publisher",
"first-page": "e1003773",
"journal-title": "PLoS Med",
"key": "key-10.3201/eid3003.231194-202402141031-R17",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1136/bmj.n1098",
"article-title": "Risk of clinical sequelae after the acute phase of SARS-CoV-2 infection: retrospective cohort study.",
"author": "Daugherty",
"doi-asserted-by": "publisher",
"first-page": "n1098",
"journal-title": "BMJ",
"key": "key-10.3201/eid3003.231194-202402141031-R18",
"volume": "373",
"year": "2021"
},
{
"DOI": "10.1371/journal.pmed.1004122",
"article-title": "Post-COVID-19-associated morbidity in children, adolescents, and adults: A matched cohort study including more than 157,000 individuals with COVID-19 in Germany.",
"author": "Roessler",
"doi-asserted-by": "publisher",
"first-page": "e1004122",
"journal-title": "PLoS Med",
"key": "key-10.3201/eid3003.231194-202402141031-R19",
"volume": "19",
"year": "2022"
},
{
"key": "key-10.3201/eid3003.231194-202402141031-R20",
"unstructured": "Institute of Medicine. Beyond myalgic encephalomyelitis/chronic fatigue syndrome: redefining an illness. Washington: The National Academies; 2015."
},
{
"key": "key-10.3201/eid3003.231194-202402141031-R21",
"unstructured": "Centers for Disease Control and Prevention. Myalgic encephalomyelitis/chronic fatigue syndrome: ICD-10-CM codes [cited 2023 Dec 15]. https://www.cdc.gov/me-cfs/healthcare-providers/diagnosis/icd-10.html"
},
{
"DOI": "10.1176/appi.ajp.2020.20060842",
"article-title": "Mood disorders and outcomes of COVID-19 hospitalizations.",
"author": "Castro",
"doi-asserted-by": "publisher",
"first-page": "541",
"journal-title": "Am J Psychiatry",
"key": "key-10.3201/eid3003.231194-202402141031-R22",
"volume": "178",
"year": "2021"
},
{
"DOI": "10.1016/j.bbi.2010.07.245",
"article-title": "Sleep depth and fatigue: role of cellular inflammatory activation.",
"author": "Thomas",
"doi-asserted-by": "publisher",
"first-page": "53",
"journal-title": "Brain Behav Immun",
"key": "key-10.3201/eid3003.231194-202402141031-R23",
"volume": "25",
"year": "2011"
},
{
"key": "key-10.3201/eid3003.231194-202402141031-R24",
"unstructured": "Washington State Department of Health. SARS-CoV-2 sequencing and variants in Washington state [cited 2023 May 5]. https://doh.wa.gov/sites/default/files/2022-02/420-316-SequencingAndVariantsReport.pdf"
},
{
"DOI": "10.1093/cid/ciad045",
"article-title": "Severe fatigue and persistent symptoms at 3 months following severe acute respiratory syndrome coronavirus 2 infections during the pre-Delta, Delta, and Omicron time periods: a multicenter prospective cohort study.",
"author": "Gottlieb",
"doi-asserted-by": "publisher",
"first-page": "1930",
"journal-title": "Clin Infect Dis",
"key": "key-10.3201/eid3003.231194-202402141031-R25",
"volume": "76",
"year": "2023"
},
{
"DOI": "10.1038/s41409-021-01419-2",
"article-title": "Clinical characterization and cytokine profile of fatigue in hematologic malignancy patients with chronic graft-versus-host disease.",
"author": "Goklemez",
"doi-asserted-by": "publisher",
"first-page": "2934",
"journal-title": "Bone Marrow Transplant",
"key": "key-10.3201/eid3003.231194-202402141031-R26",
"volume": "56",
"year": "2021"
}
],
"reference-count": 26,
"references-count": 26,
"relation": {},
"resource": {
"primary": {
"URL": "https://wwwnc.cdc.gov/eid/article/30/3/23-1194_article"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Infectious Diseases",
"Microbiology (medical)",
"Epidemiology"
],
"subtitle": [],
"title": "Estimates of Incidence and Predictors of Fatiguing Illness after SARS-CoV-2 Infection",
"type": "journal-article",
"volume": "30"
}
