Association of Gastric Acid Suppression With Recurrent Clostridium difficile Infection
et al., JAMA Internal Medicine, doi:10.1001/jamainternmed.2017.0212, Jun 2017
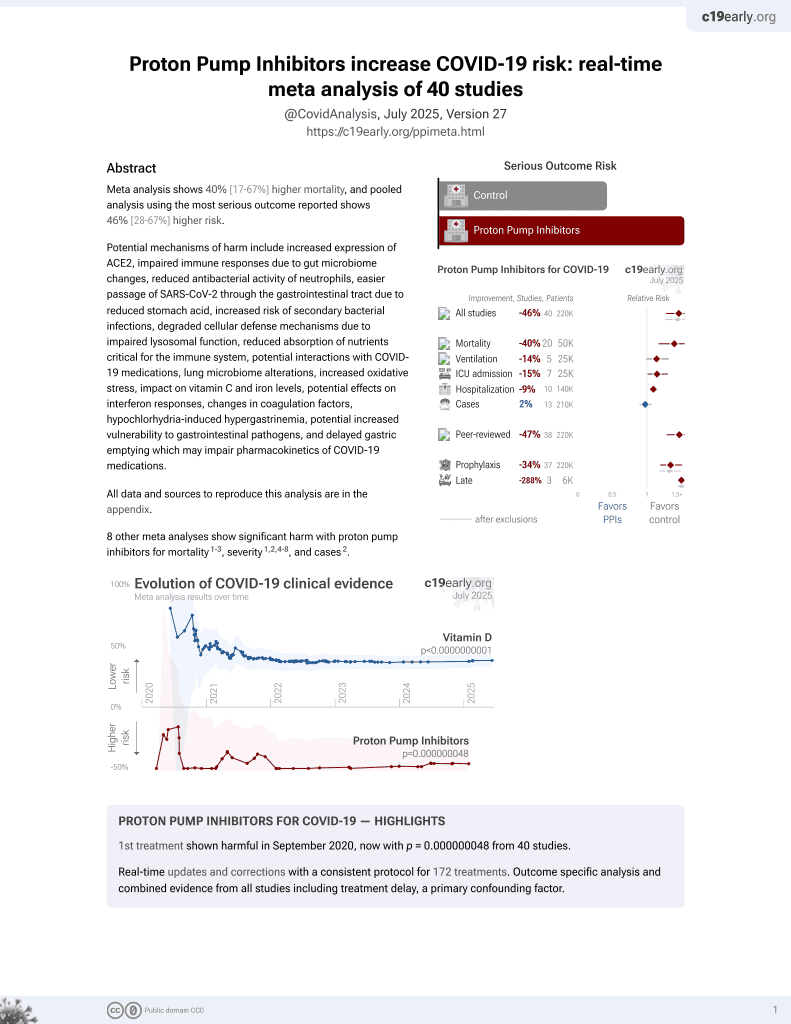
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
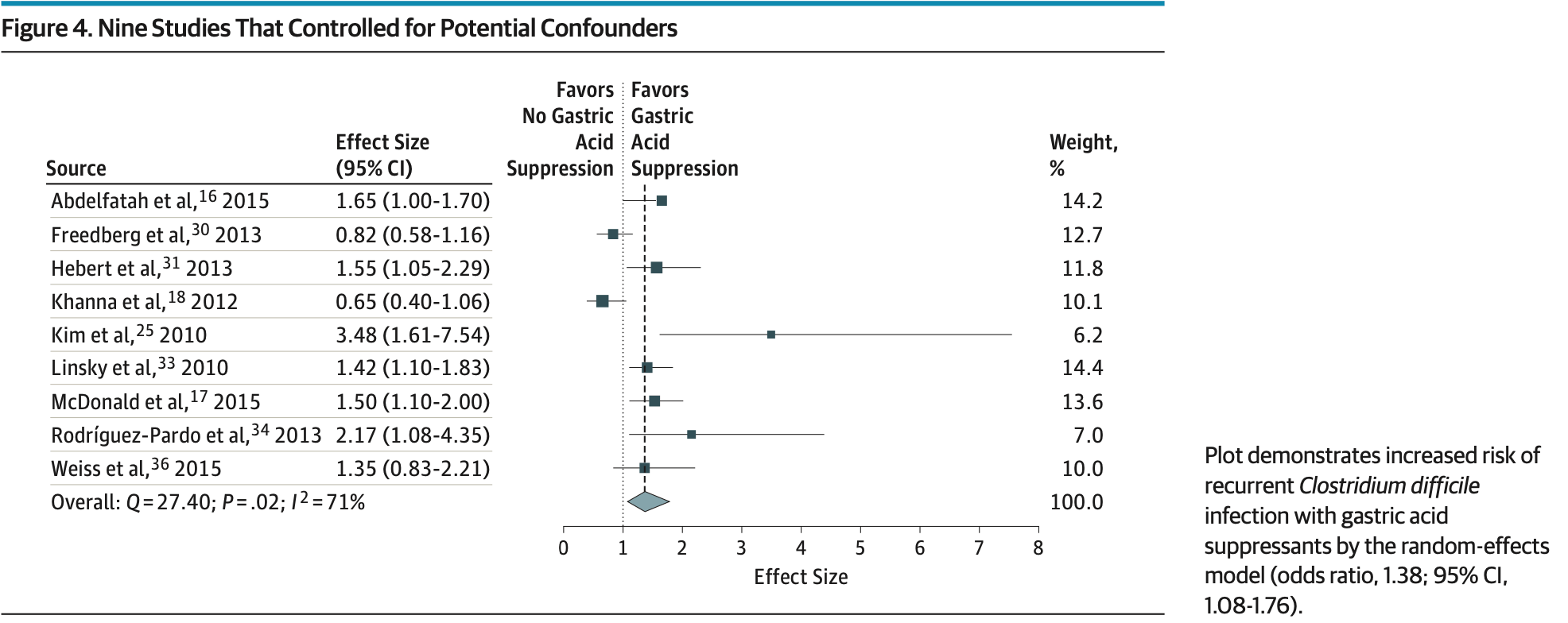
Meta-analysis of 16 observational studies with 7,703 patients showing increased risk of recurrent C. difficile infection with gastric acid suppressant use (PPIs alone or PPIs/H2RAs).
Tariq et al., 1 Jun 2017, peer-reviewed, 5 authors.
Contact: khanna.sahil@mayo.edu.
Association of Gastric Acid Suppression With Recurrent Clostridium difficile Infection
JAMA Internal Medicine, doi:10.1001/jamainternmed.2017.0212
IMPORTANCE Gastric acid suppression has been associated with an increased risk of primary Clostridium difficile infection (CDI), but the risk of recurrent CDI in patients taking gastric acid suppressant medications is unclear. OBJECTIVE To perform a systematic review and meta-analysis to evaluate the association between gastric acid suppressants and recurrent CDI. DATA SOURCES MEDLINE, EMBASE, the Cochrane Central Register, the Cochrane Database, and Web of Science were searched from January 1, 1995, to September 30, 2015, for studies assessing the association between gastric acid suppressant exposure and recurrent CDI. Search terms included Clostridium difficile, pseudomembranous colitis, proton pump inhibitor, and histamine H 2 blocker. STUDY SELECTION Case-control studies, cohort studies, and clinical trials that included patients with CDI who did or did not receive gastric acid suppressant therapy and who were evaluated for recurrent CDI were included, with no restriction on study setting (inpatient or outpatient).
DATA EXTRACTION AND SYNTHESIS The Newcastle-Ottawa scale was used to assess the methodologic quality of included studies. In this scale, case-control and cohort studies were scored on selection, comparability, and ascertainment of the outcome of interest. Data were independently abstracted to a predetermined collection form by 2 investigators. Summary odds ratio estimates with 95% CIs were calculated using the random-effects model and software to calculate the pooled effect size of studies reporting multivariate analyses. MAIN OUTCOMES AND MEASURES Risk of recurrent infection in patients with CDI and its association with use of gastric acid suppressant medication.
RESULTS Sixteen observational studies were included, together reporting 7703 patients with CDI; among these, 1525 patients (19.8%) developed recurrent CDI. The rate of recurrent CDI in patients with gastric acid suppression was 22.1% (892 of 4038 patients) compared with 17.3% (633 of 3665) in patients without gastric acid suppression, which indicated an increased risk by meta-analysis (odds ratio [OR], 1.52; 95% CI, 1.20-1.94; P < .001). There was significant heterogeneity among the studies, with an I 2 value of 64%. Subgroup analyses of studies adjusting for age and potential confounders confirmed an increased risk of recurrent CDI with use of gastric acid suppressants (OR, 1.38; 95% CI, 1.08-1.76; P = .02). CONCLUSIONS AND RELEVANCE Meta-analyses of observational studies suggest that patients who receive gastric acid suppressants may be at increased risk for recurrent CDI. These data should be interpreted with caution because they may be confounded owing to the observational design of the individual studies. It may be reasonable to re-evaluate the need for these medications in patients with CDI.
References
Abdelfatah, Nayfe, Nijim, Factors predicting recurrence of Clostridium difficile infection (CDI) in hospitalized patients: retrospective study of more than 2,000 patients, J Investig Med
Cadena, Thompson, Iii, Patterson, Clinical predictors and risk factors for relapsing Clostridium difficile infection, Am J Med Sci
Cadle, Mansouri, Logan, Kudva, Musher, Association of proton-pump inhibitors with outcomes in Clostridium difficile colitis, Am J Health Syst Pharm
Choudhry, Soran, Ziglam, Overuse and inappropriate prescribing of proton pump inhibitors in patients with Clostridium difficile-associated disease, QJM
Cohen, Gerding, Johnson, Society for Healthcare Epidemiology of America; Infectious Diseases Society of America. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA), Infect Control Hosp Epidemiol
Dersimonian, Laird, Meta-analysis in clinical trials, Control Clin Trials
Deshpande, Pasupuleti, Thota, Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis, Infect Control Hosp Epidemiol
Easterbrook, Berlin, Gopalan, Matthews, Publication bias in clinical research, Lancet
Freedberg, Salmasian, Friedman, Abrams, Proton pump inhibitors and risk for recurrent Clostridium difficile infection among inpatients, Am J Gastroenterol
Hebert, Du, Peterson, Robicsek, Electronic health record-based detection of risk factors for Clostridium difficile infection relapse, Infect Control Hosp Epidemiol
Hikone, Ainoda, Tago, Risk factors for recurrent hospital-acquired Clostridium difficile infection in a Japanese university hospital, Clin Exp Gastroenterol
Hu, Katchar, Kyne, Prospective derivation and validation of a clinical prediction rule for recurrent Clostridium difficile infection, Gastroenterology
Imhann, Bonder, Vila, Proton pump inhibitors affect the gut microbiome, Gut
Jackson, Goodrich, Maxan, Proton pump inhibitors alter the composition of the gut microbiota, Gut
Janarthanan, Ditah, Adler, Ehrinpreis, Clostridium difficile-associated diarrhea and proton pump inhibitor therapy: a meta-analysis, Am J Gastroenterol
Keddis, Khanna, Noheria, Baddour, Pardi et al., Clostridium difficile infection in patients with chronic kidney disease, Mayo Clin Proc
Khanna, Aronson, Kammer, Baddour, Pardi, Gastric acid suppression and outcomes in Clostridium difficile infection: a population-based study, Mayo Clin Proc
Khanna, Pardi, Aronson, The epidemiology of community-acquired Clostridium difficile infection: a population-based study, Am J Gastroenterol
Khanna, Pardi, Clostridium difficile infection: management strategies for a difficult disease, Therap Adv Gastroenterol
Khanna, Pardi, Clostridium difficile infection: new insights into management, Mayo Clin Proc
Khanna, Pardi, Gastric acid suppression and Clostridium difficile infection: is there a causal connection?, Clin Gastroenterol Hepatol
Khanna, Pardi, The growing incidence and severity of Clostridium difficile infection in inpatient and outpatient settings, Expert Rev Gastroenterol Hepatol
Kim, Graham, Jang, Proton pump inhibitor use and recurrent Clostridium difficile-associated disease: a case-control analysis matched by propensity score, J Clin Gastroenterol
Kim, Lee, Jeong, Proton pump inhibitors as a risk factor for recurrence of Clostridium-difficile-associated diarrhea, World J Gastroenterol
Kwok, Arthur, Anibueze, Singh, Cavallazzi et al., Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis, Am J Gastroenterol
Kyne, Sougioultzis, Mcfarland, Kelly, Underlying disease severity as a major risk factor for nosocomial Clostridium difficile diarrhea, Infect Control Hosp Epidemiol
Kyne, Warny, Qamar, Kelly, Association between antibody response to toxin A and protection against recurrent Clostridium difficile diarrhoea, Lancet
Leonard, Marshall, Moayyedi, Systematic review of the risk of enteric infection in patients taking acid suppression, Am J Gastroenterol
Lessa, Winston, Mcdonald, Emerging Infections Program C difficile Surveillance Team. Burden of Clostridium difficile infection in the United States, N Engl J Med
Linsky, Gupta, Lawler, Fonda, Hermos, Proton pump inhibitors and risk for recurrent Clostridium difficile infection, Arch Intern Med
Magill, Edwards, Bamberg, Emerging Infections Program Healthcare-Associated Infections and Antimicrobial Use Prevalence Survey Team. Multistate point-prevalence survey of health care-associated infections, N Engl J Med
Mcdonald, Milligan, Frenette, Lee, Continuous proton pump inhibitor therapy and the associated risk of recurrent Clostridium difficile infection, JAMA Intern Med
Moher, Liberati, Tetzlaff, Altman, Group, Preferred Reporting Items for Systematic reviews and Meta-Analyses: the PRISMA statement, PLoS Med
Moshkowitz, Ben-Baruch, Kline, Shimoni, Niven et al., Risk factors for severity and relapse of pseudomembranous colitis in an elderly population, Colorectal Dis
Owens Rc, Donskey, Gaynes, Loo, Muto, Antimicrobial-associated risk factors for Clostridium difficile infection, Clin Infect Dis
Pépin, Saheb, Coulombe, Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec, Clin Infect Dis
Rodríguez-Pardo, Almirante, Bartolomé, Epidemiology of Clostridium difficile infection and risk factors for unfavorable clinical outcomes: results of a hospital-based study in Barcelona, Spain, J Clin Microbiol
Samie, Traub, Bachmann, Kopischke, Theilmann, Risk factors for recurrence of Clostridium difficile-associated diarrhoea, Hepatogastroenterology
Scott, Bauer, Scm, Patrick, Malley et al., s Note Withholding Proton Pump Inhibitors to Prevent Recurrent Clostridium difficile Time for a Randomized Trial
Shivashankar, Khanna, Kammer, Clinical factors associated with development of severe-complicated Clostridium difficile infection, Clin Gastroenterol Hepatol
Stroup, Berlin, Morton, Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. Meta-analysis of observational studies in epidemiology: a proposal for reporting, JAMA
Tal, Gurevich, Guller, Gurevich, Berger et al., Risk factors for recurrence of Clostridium difficile-associated diarrhea in the elderly, Scand J Infect Dis
Weiss, Louie, Miller, Mullane, Crook et al., Effects of proton pump inhibitors and histamine-2 receptor antagonists on response to fidaxomicin or vancomycin in patients with Clostridium difficile-associated diarrhoea, BMJ Open Gastroenterol
Wells, Shea, Connell, The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses
DOI record:
{
"DOI": "10.1001/jamainternmed.2017.0212",
"ISSN": [
"2168-6106"
],
"URL": "http://dx.doi.org/10.1001/jamainternmed.2017.0212",
"author": [
{
"affiliation": [
{
"name": "Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota"
}
],
"family": "Tariq",
"given": "Raseen",
"sequence": "first"
},
{
"affiliation": [
{
"name": "Division of Gastroenterology and Hepatology, University of California, San Diego, La Jolla"
}
],
"family": "Singh",
"given": "Siddharth",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Infectious Diseases, Mayo Clinic, Rochester, Minnesota"
}
],
"family": "Gupta",
"given": "Arjun",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota"
}
],
"family": "Pardi",
"given": "Darrell S.",
"sequence": "additional"
},
{
"affiliation": [
{
"name": "Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota"
}
],
"family": "Khanna",
"given": "Sahil",
"sequence": "additional"
}
],
"container-title": "JAMA Internal Medicine",
"container-title-short": "JAMA Intern Med",
"content-domain": {
"crossmark-restriction": false,
"domain": []
},
"created": {
"date-parts": [
[
2017,
3,
28
]
],
"date-time": "2017-03-28T00:38:46Z",
"timestamp": 1490661526000
},
"deposited": {
"date-parts": [
[
2018,
2,
2
]
],
"date-time": "2018-02-02T20:31:16Z",
"timestamp": 1517603476000
},
"indexed": {
"date-parts": [
[
2024,
8,
24
]
],
"date-time": "2024-08-24T02:28:58Z",
"timestamp": 1724466538000
},
"is-referenced-by-count": 111,
"issue": "6",
"issued": {
"date-parts": [
[
2017,
6,
1
]
]
},
"journal-issue": {
"issue": "6",
"published-print": {
"date-parts": [
[
2017,
6,
1
]
]
}
},
"language": "en",
"link": [
{
"URL": "http://archinte.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2017.0212",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "10",
"original-title": [],
"page": "784",
"prefix": "10.1001",
"published": {
"date-parts": [
[
2017,
6,
1
]
]
},
"published-print": {
"date-parts": [
[
2017,
6,
1
]
]
},
"publisher": "American Medical Association (AMA)",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://archinte.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2017.0212"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [
"A Systematic Review and Meta-analysis"
],
"title": "Association of Gastric Acid Suppression With Recurrent <i>Clostridium difficile</i> Infection",
"type": "journal-article",
"volume": "177"
}