The F/B ratio as a biomarker for inflammation in COVID-19 and T2D: Impact of metformin
et al., Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2023.114892, May 2023
Metformin for COVID-19
3rd treatment shown to reduce risk in
July 2020, now with p < 0.00000000001 from 110 studies.
Lower risk for mortality, ventilation, ICU, hospitalization, progression, recovery, and viral clearance.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
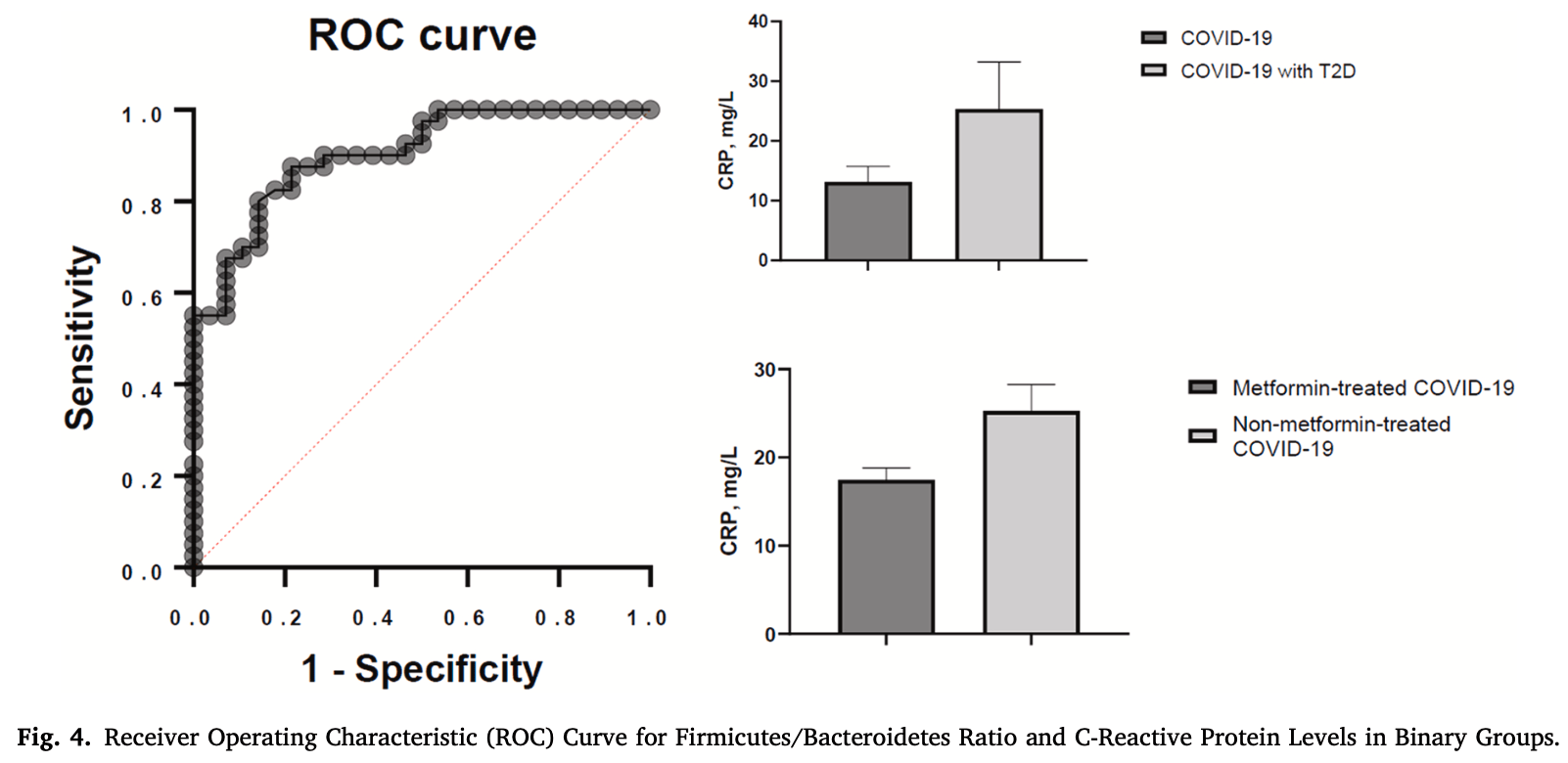
Analysis of 115 pateints in Ukraine, providing evidence that the gut microbiome may play a role in the inflammatory response of COVID-19 patients, that the firmicutes/bacteroidetes ratio may be a potential biomarker for inflammation, and that metformin may affect the relationship between the firmicutes/bacteroidetes ratio and CRP levels.
Petakh et al., 15 May 2023, Ukraine, peer-reviewed, 3 authors.
Contact: pavlo.petakh@uzhnu.edu.ua, alexkamyshnyi@gmail.com.
The F/B ratio as a biomarker for inflammation in COVID-19 and T2D: Impact of metformin
Biomedicine & Pharmacotherapy, doi:10.1016/j.biopha.2023.114892
The pandemic of COVID-19 has highlighted the intricate relationship between gut microbiome and overall health. Recent studies have shown that the Firmicutes/Bacteroidetes ratio in the gut microbiome may be linked to various diseases including COVID-19 and type 2 diabetes (T2D). Understanding the link between gut microbiome and these diseases is essential for developing strategies for prevention and treatment. In this study, 115 participants were recruited and divided into three groups: 1st group: T2D patients and healthy controls, 2nd group: COVID-19 patients with and without T2D, 3rd group: T2D patients with COVID-19 treated with or without metformin. Gut microbial composition at the phylum level was assessed using qRT-PCR with universal primers targeting the bacterial 16 S rRNA gene and specific primers for Firmicutes and Bacteroidetes. Data was analyzed using one-way ANOVA, logistic regression, and Spearman's rank correlation coefficient. The study found that the ratio of Firmicutes to Bacteroidetes (F/B) was higher in patients with both T2D and COVID-19 compared to those with only T2D or COVID-19. Additionally, the F/B ratio was positively correlated with Creactive protein (CRP) in T2D and COVID-19 patients. The study also suggests that metformin treatment may affect this correlation. Logistic regression analysis showed that the F/B ratio was significantly associated with CRP. These findings suggest that the F/B ratio may be a potential biomarker for inflammation in T2D and COVID-19 patients and metformin treatment may have an effect on the correlation between F/B and CRP levels.
Conflicts of Interest The authors declare no conflict of interest.
Declaration of Competing Interest The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
An, Kwon, Kim, The firmicutes/bacteroidetes ratio as a risk factor of breast cancer, J. Clin. Med
Bacchetti De Gregoris, Aldred, Clare, Burgess, Improvement of phylum-and class-specific primers for real-time PCR quantification of bacterial taxa, J. Microbiol. Methods
Bailey, Gwilt, None, Diabetes, Metformin Clin. Course Covid-19: Outcomes, Mech. Suggest. Ther. Use Metformin
Bouayed, Laaribi, Chatar, Benaini, Bouazzaoui et al., C-Reactive Protein (CRP): a poor prognostic biomarker in COVID-19, Front. Immunol
Burchill, Lymberopoulos, Menozzi, Budhdeo, Mcilroy et al., The unique impact of COVID-19 on human gut microbiome research, Front. Med
Chen, Guo, Qiu, Zhang, Deng et al., Immunomodulatory and antiviral activity of metformin and its potential implications in treating coronavirus disease 2019 and lung injury, Front Immunol
Chen, Vitetta, Modulation of gut microbiota for the prevention and treatment of COVID-19, J. Clin. Med
Chávez-Carbajal, Pizano-Zárate, Hernández-Quiroz, Ortiz-Luna, Morales-Hernández et al., Characterization of the gut microbiota of individuals at different T2D stages reveals a complex relationship with the host
Cunningham, Stephens, Harris, Gut microbiota influence in type 2 diabetes mellitus (T2DM)
Forslund, Hildebrand, Nielsen, Falony, Le Chatelier et al., Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota, Nature
Gradisteanu Pircalabioru, Grigore, Czobor, Barbu, Chifiriuc et al., Impact of COVID-19 on the microbiome and inflammatory status of type 2 diabetes patients, Biomedicines
Hung, Hung, Tsai, Chang, Chiu et al., The association of targeted gut microbiota with body composition in type 2 diabetes mellitus, Int. J. Med. Sci
Ibrahim, Lowe, Bramante, Shah, Klatt et al., Metformin and Covid-19: focused review of mechanisms and current literature suggesting benefit, Front Endocrinol. (Lausanne)
Jasirwan, Muradi, Hasan, Simadibrata, Rinaldi, Correlation of gut Firmicutes/Bacteroidetes ratio with fibrosis and steatosis stratified by body mass index in patients with non-alcoholic fatty liver disease, Biosci. Micro, Food Health
Kamyshnyi, Matskevych, Lenchuk, Strilbytska, Storey et al., Metformin to decrease COVID-19 severity and mortality: molecular mechanisms and therapeutic potential, Biomed. Pharmacother
Khan, Mathew, Gupta, Garg, Khadanga et al., Gut dysbiosis and IL-21 response in patients with severe COVID-19, Microorganisms
Lambeth, Carson, Lowe, Ramaraj, Leff et al., Composition, diversity and abundance of gut microbiome in prediabetes and type 2 diabetes, J. Diabetes Obes
Larsen, Vogensen, Van Den, Berg, Nielsen et al., Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults, PLoS One
Lentner, Adams, Knutson, Zeien, Abbas et al., C-reactive protein levels associated with COVID-19 outcomes in the United States, J. Osteopath. Med
Liu, Bei, Liang, Yu, Li et al., Stachyose improves inflammation through modulating gut microbiota of high-fat diet/streptozotocin-induced type 2 diabetes in rats, Mol. Nutr. Food Res
Magne, Gotteland, Gauthier, Zazueta, Pesoa et al., The firmicutes/bacteroidetes ratio: a relevant marker of gut dysbiosis in obese patients?, Nutrients
Oren, Garrity, Valid publication of the names of forty-two phyla of prokaryotes
Parthasarathy, Tandel, Siddiqui, Harshan, Metformin suppresses SARS-CoV-2 in cell culture, Virus Res
Petakh, Griga, Mohammed, Loshak, Poliak et al., Effects of metformin, insulin on hematological parameters of COVID-19 patients with type 2 diabetes, Med. Arch
Petakh, Isevych, Mohammed, Loshak, Poliak et al., Association between use of metformin and insulin with hematological parameters in COVID-19 patients with type 2 diabetes: a single center, cross-sectional study, Clin. Diabetol
Petakh, Kamyshna, Nykyforuk, Yao, Imbery et al., Immunoregulatory intestinal microbiota and COVID-19 in patients with type two diabetes: a double-edged sword, J. Virus
Petakh, Kobyliak, Kamyshnyi, Gut microbiota in patients with COVID-19 and type 2 diabetes: a culture-based method, Front. Cell. Infect. Microbiol
Reitmeier, Kiessling, Clavel, List, Almeida et al., Arrhythmic gut microbiome signatures predict risk of type 2 diabetes, Cell Host Microbe
Sedighi, Razavi, Navab-Moghadam, Khamseh, Alaei-Shahmiri et al., Comparison of gut microbiota in adult patients with type 2 diabetes and healthy individuals, Microb. Pathog
Stojanov, Berlec, Štrukelj, The influence of probiotics on the firmicutes/ bacteroidetes ratio in the treatment of obesity and inflammatory bowel disease, Microorganisms
Takezawa, Fujita, Matsushita, Motooka, Hatano et al., The Firmicutes/Bacteroidetes ratio of the human gut microbiota is associated with prostate enlargement, Prostate
Targher, Mantovani, Wang, Yan, Sun et al., Patients with diabetes are at higher risk for severe illness from COVID-19, Diabetes Metab
Yeoh, Zuo, Lui, Zhang, Liu et al., Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19, Gut
Zhang, Hu, Metabolic syndrome, targets O, therapy. Effects of metformin on the gut microbiota in obesity and type 2 diabetes mellitus, Diabetes Metad. Syndr. Obes
Zhao, Lou, Peng, Chen, Zhang et al., Comprehensive relationships between gut microbiome and faecal metabolome in individuals with type 2 diabetes and its complications, Endocrine
DOI record:
{
"DOI": "10.1016/j.biopha.2023.114892",
"ISSN": [
"0753-3322"
],
"URL": "http://dx.doi.org/10.1016/j.biopha.2023.114892",
"alternative-id": [
"S0753332223006820"
],
"article-number": "114892",
"assertion": [
{
"label": "This article is maintained by",
"name": "publisher",
"value": "Elsevier"
},
{
"label": "Article Title",
"name": "articletitle",
"value": "The F/B ratio as a biomarker for inflammation in COVID-19 and T2D: Impact of metformin"
},
{
"label": "Journal Title",
"name": "journaltitle",
"value": "Biomedicine & Pharmacotherapy"
},
{
"label": "CrossRef DOI link to publisher maintained version",
"name": "articlelink",
"value": "https://doi.org/10.1016/j.biopha.2023.114892"
},
{
"label": "Content Type",
"name": "content_type",
"value": "article"
},
{
"label": "Copyright",
"name": "copyright",
"value": "© 2023 The Author(s). Published by Elsevier Masson SAS."
}
],
"author": [
{
"ORCID": "http://orcid.org/0000-0002-0860-4445",
"affiliation": [],
"authenticated-orcid": false,
"family": "Petakh",
"given": "Pavlo",
"sequence": "first"
},
{
"affiliation": [],
"family": "Oksenych",
"given": "Valentyn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Kamyshnyi",
"given": "Aleksandr",
"sequence": "additional"
}
],
"container-title": "Biomedicine & Pharmacotherapy",
"container-title-short": "Biomedicine & Pharmacotherapy",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"clinicalkey.fr",
"clinicalkey.jp",
"clinicalkey.es",
"clinicalkey.com.au",
"clinicalkey.com",
"em-consulte.com",
"elsevier.com",
"sciencedirect.com"
]
},
"created": {
"date-parts": [
[
2023,
5,
15
]
],
"date-time": "2023-05-15T17:28:17Z",
"timestamp": 1684171697000
},
"deposited": {
"date-parts": [
[
2023,
5,
15
]
],
"date-time": "2023-05-15T19:50:55Z",
"timestamp": 1684180255000
},
"indexed": {
"date-parts": [
[
2023,
5,
16
]
],
"date-time": "2023-05-16T04:39:39Z",
"timestamp": 1684211979825
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
7
]
]
},
"language": "en",
"license": [
{
"URL": "https://www.elsevier.com/tdm/userlicense/1.0/",
"content-version": "tdm",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
7,
1
]
],
"date-time": "2023-07-01T00:00:00Z",
"timestamp": 1688169600000
}
},
{
"URL": "http://creativecommons.org/licenses/by-nc-nd/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
14
]
],
"date-time": "2023-05-14T00:00:00Z",
"timestamp": 1684022400000
}
}
],
"link": [
{
"URL": "https://api.elsevier.com/content/article/PII:S0753332223006820?httpAccept=text/xml",
"content-type": "text/xml",
"content-version": "vor",
"intended-application": "text-mining"
},
{
"URL": "https://api.elsevier.com/content/article/PII:S0753332223006820?httpAccept=text/plain",
"content-type": "text/plain",
"content-version": "vor",
"intended-application": "text-mining"
}
],
"member": "78",
"original-title": [],
"page": "114892",
"prefix": "10.1016",
"published": {
"date-parts": [
[
2023,
7
]
]
},
"published-print": {
"date-parts": [
[
2023,
7
]
]
},
"publisher": "Elsevier BV",
"reference": [
{
"DOI": "10.3389/fmed.2021.652464",
"article-title": "The unique impact of COVID-19 on human gut microbiome research",
"author": "Burchill",
"doi-asserted-by": "crossref",
"journal-title": "Front. Med.",
"key": "10.1016/j.biopha.2023.114892_bib1",
"volume": "8",
"year": "2021"
},
{
"DOI": "10.3390/v14030477",
"article-title": "Immunoregulatory intestinal microbiota and COVID-19 in patients with type two diabetes: a double-edged sword",
"author": "Petakh",
"doi-asserted-by": "crossref",
"first-page": "477",
"issue": "3",
"journal-title": "J. Virus",
"key": "10.1016/j.biopha.2023.114892_bib2",
"volume": "14",
"year": "2022"
},
{
"DOI": "10.3390/microorganisms9061292",
"article-title": "Gut dysbiosis and IL-21 response in patients with severe COVID-19",
"author": "Khan",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Microorganisms",
"key": "10.1016/j.biopha.2023.114892_bib3",
"volume": "9",
"year": "2021"
},
{
"DOI": "10.1186/s13099-021-00446-0",
"article-title": "Gut microbiota influence in type 2 diabetes mellitus (T2DM)",
"author": "Cunningham",
"doi-asserted-by": "crossref",
"first-page": "50",
"issue": "1",
"journal-title": "Gut Pathog.",
"key": "10.1016/j.biopha.2023.114892_bib4",
"volume": "13",
"year": "2021"
},
{
"DOI": "10.3390/jcm10132903",
"article-title": "Modulation of gut microbiota for the prevention and treatment of COVID-19",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "2903",
"issue": "13",
"journal-title": "J. Clin. Med.",
"key": "10.1016/j.biopha.2023.114892_bib5",
"volume": "10",
"year": "2021"
},
{
"article-title": "Valid publication of the names of forty-two phyla of prokaryotes",
"author": "Oren",
"issue": "10",
"key": "10.1016/j.biopha.2023.114892_bib6",
"volume": "71",
"year": "2021"
},
{
"DOI": "10.1016/j.diabet.2020.05.001",
"article-title": "Patients with diabetes are at higher risk for severe illness from COVID-19",
"author": "Targher",
"doi-asserted-by": "crossref",
"first-page": "335",
"issue": "4",
"journal-title": "Diabetes Metab.",
"key": "10.1016/j.biopha.2023.114892_bib7",
"volume": "46",
"year": "2020"
},
{
"DOI": "10.3390/biomedicines11010179",
"article-title": "Impact of COVID-19 on the microbiome and inflammatory status of type 2 diabetes patients",
"author": "Gradisteanu Pircalabioru",
"doi-asserted-by": "crossref",
"first-page": "179",
"issue": "1",
"journal-title": "Biomedicines",
"key": "10.1016/j.biopha.2023.114892_bib8",
"volume": "11",
"year": "2023"
},
{
"DOI": "10.3389/fcimb.2023.1142578",
"article-title": "Gut microbiota in patients with COVID-19 and type 2 diabetes: a culture-based method",
"author": "Petakh",
"doi-asserted-by": "crossref",
"journal-title": "Front. Cell. Infect. Microbiol.",
"key": "10.1016/j.biopha.2023.114892_bib9",
"volume": "13",
"year": "2023"
},
{
"DOI": "10.7150/ijms.51164",
"article-title": "The association of targeted gut microbiota with body composition in type 2 diabetes mellitus",
"author": "Hung",
"doi-asserted-by": "crossref",
"first-page": "511",
"issue": "2",
"journal-title": "Int. J. Med. Sci.",
"key": "10.1016/j.biopha.2023.114892_bib10",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.3390/nu12051474",
"article-title": "The firmicutes/bacteroidetes ratio: a relevant marker of gut dysbiosis in obese patients?",
"author": "Magne",
"doi-asserted-by": "crossref",
"issue": "5",
"journal-title": "Nutrients",
"key": "10.1016/j.biopha.2023.114892_bib11",
"volume": "12",
"year": "2020"
},
{
"DOI": "10.1136/gutjnl-2020-323020",
"article-title": "Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19",
"author": "Yeoh",
"doi-asserted-by": "crossref",
"first-page": "698",
"issue": "4",
"journal-title": "Gut",
"key": "10.1016/j.biopha.2023.114892_bib12",
"volume": "70",
"year": "2021"
},
{
"DOI": "10.3389/fimmu.2022.1040024",
"article-title": "C-Reactive Protein (CRP): a poor prognostic biomarker in COVID-19",
"author": "Bouayed",
"doi-asserted-by": "crossref",
"journal-title": "Front. Immunol.",
"key": "10.1016/j.biopha.2023.114892_bib13",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1515/jom-2021-0103",
"article-title": "C-reactive protein levels associated with COVID-19 outcomes in the United States.",
"author": "Lentner",
"doi-asserted-by": "crossref",
"first-page": "869",
"issue": "12",
"journal-title": "J. Osteopath. Med.",
"key": "10.1016/j.biopha.2023.114892_bib14",
"volume": "121",
"year": "2021"
},
{
"DOI": "10.2337/dc22-S002",
"doi-asserted-by": "crossref",
"key": "10.1016/j.biopha.2023.114892_bib15",
"unstructured": "2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17-s38."
},
{
"key": "10.1016/j.biopha.2023.114892_bib16",
"unstructured": "[Available from: 〈https://www.thermofisher.com/order/catalog/product/10503027〉."
},
{
"DOI": "10.1016/j.mimet.2011.06.010",
"article-title": "Improvement of phylum- and class-specific primers for real-time PCR quantification of bacterial taxa",
"author": "Bacchetti De Gregoris",
"doi-asserted-by": "crossref",
"first-page": "351",
"issue": "3",
"journal-title": "J. Microbiol. Methods",
"key": "10.1016/j.biopha.2023.114892_bib17",
"volume": "86",
"year": "2011"
},
{
"DOI": "10.1371/journal.pone.0009085",
"article-title": "Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults",
"author": "Larsen",
"doi-asserted-by": "crossref",
"issue": "2",
"journal-title": "PLoS One",
"key": "10.1016/j.biopha.2023.114892_bib18",
"volume": "5",
"year": "2010"
},
{
"DOI": "10.1016/j.micpath.2017.08.038",
"article-title": "Comparison of gut microbiota in adult patients with type 2 diabetes and healthy individuals",
"author": "Sedighi",
"doi-asserted-by": "crossref",
"first-page": "362",
"journal-title": "Microb. Pathog.",
"key": "10.1016/j.biopha.2023.114892_bib19",
"volume": "111",
"year": "2017"
},
{
"DOI": "10.1007/s12020-019-02103-8",
"article-title": "Comprehensive relationships between gut microbiome and faecal metabolome in individuals with type 2 diabetes and its complications",
"author": "Zhao",
"doi-asserted-by": "crossref",
"first-page": "526",
"issue": "3",
"journal-title": "Endocrine",
"key": "10.1016/j.biopha.2023.114892_bib20",
"volume": "66",
"year": "2019"
},
{
"article-title": "Composition, diversity and abundance of gut microbiome in prediabetes and type 2 diabetes",
"author": "Lambeth",
"first-page": "1",
"issue": "3",
"journal-title": "J. Diabetes Obes.",
"key": "10.1016/j.biopha.2023.114892_bib21",
"volume": "2",
"year": "2015"
},
{
"DOI": "10.1016/j.chom.2020.06.004",
"article-title": "Arrhythmic gut microbiome signatures predict risk of type 2 diabetes",
"author": "Reitmeier",
"doi-asserted-by": "crossref",
"first-page": "258",
"issue": "2",
"journal-title": "Cell Host Microbe",
"key": "10.1016/j.biopha.2023.114892_bib22",
"volume": "28",
"year": "2020"
},
{
"DOI": "10.5455/medarh.2022.76.329-332",
"article-title": "Effects of metformin, insulin on hematological parameters of COVID-19 patients with type 2 diabetes",
"author": "Petakh",
"doi-asserted-by": "crossref",
"first-page": "329",
"issue": "5",
"journal-title": "Med. Arch.",
"key": "10.1016/j.biopha.2023.114892_bib23",
"volume": "76",
"year": "2022"
},
{
"DOI": "10.5603/DK.a2022.0055",
"article-title": "Association between use of metformin and insulin with hematological parameters in COVID-19 patients with type 2 diabetes: a single center, cross-sectional study",
"author": "Petakh",
"doi-asserted-by": "crossref",
"first-page": "432",
"issue": "6",
"journal-title": "Clin. Diabetol.",
"key": "10.1016/j.biopha.2023.114892_bib24",
"volume": "11",
"year": "2022"
},
{
"author": "Bailey",
"journal-title": "Diabetes, Metformin Clin. Course Covid-19: Outcomes, Mech. Suggest. Ther. Use Metformin",
"key": "10.1016/j.biopha.2023.114892_bib25",
"volume": "13",
"year": "2022"
},
{
"DOI": "10.1016/j.biopha.2021.112230",
"article-title": "Metformin to decrease COVID-19 severity and mortality: molecular mechanisms and therapeutic potential",
"author": "Kamyshnyi",
"doi-asserted-by": "crossref",
"journal-title": "Biomed. Pharmacother.",
"key": "10.1016/j.biopha.2023.114892_bib26",
"volume": "144",
"year": "2021"
},
{
"DOI": "10.3389/fendo.2021.587801",
"article-title": "Metformin and Covid-19: focused review of mechanisms and current literature suggesting benefit",
"author": "Ibrahim",
"doi-asserted-by": "crossref",
"journal-title": "Front Endocrinol. (Lausanne)",
"key": "10.1016/j.biopha.2023.114892_bib27",
"volume": "12",
"year": "2021"
},
{
"article-title": "Metformin suppresses SARS-CoV-2 in cell culture",
"author": "Parthasarathy",
"journal-title": "Virus Res.",
"key": "10.1016/j.biopha.2023.114892_bib28",
"volume": "323",
"year": "2022"
},
{
"DOI": "10.3389/fimmu.2020.02056",
"article-title": "Immunomodulatory and antiviral activity of metformin and its potential implications in treating coronavirus disease 2019 and lung injury",
"author": "Chen",
"doi-asserted-by": "crossref",
"first-page": "2056",
"journal-title": "Front Immunol.",
"key": "10.1016/j.biopha.2023.114892_bib29",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.2147/DMSO.S286430",
"article-title": "Metabolic syndrome, targets O, therapy. Effects of metformin on the gut microbiota in obesity and type 2 diabetes mellitus",
"author": "Zhang",
"doi-asserted-by": "crossref",
"first-page": "5003",
"journal-title": "Diabetes Metad. Syndr. Obes.",
"key": "10.1016/j.biopha.2023.114892_bib30",
"volume": "13",
"year": "2020"
},
{
"DOI": "10.1038/nature15766",
"article-title": "Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota",
"author": "Forslund",
"doi-asserted-by": "crossref",
"first-page": "262",
"issue": "7581",
"journal-title": "Nature",
"key": "10.1016/j.biopha.2023.114892_bib31",
"volume": "528",
"year": "2015"
},
{
"DOI": "10.3390/microorganisms8010094",
"article-title": "Characterization of the gut microbiota of individuals at different T2D stages reveals a complex relationship with the host",
"author": "Chávez-Carbajal",
"doi-asserted-by": "crossref",
"first-page": "94",
"issue": "1",
"journal-title": "Microorganisms",
"key": "10.1016/j.biopha.2023.114892_bib32",
"volume": "8",
"year": "2020"
},
{
"DOI": "10.1002/mnfr.201700954",
"article-title": "Stachyose improves inflammation through modulating gut microbiota of high-fat diet/streptozotocin-induced type 2 diabetes in rats",
"author": "Liu",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "Mol. Nutr. Food Res.",
"key": "10.1016/j.biopha.2023.114892_bib33",
"volume": "62",
"year": "2018"
},
{
"DOI": "10.1002/pros.24223",
"article-title": "The Firmicutes/Bacteroidetes ratio of the human gut microbiota is associated with prostate enlargement",
"author": "Takezawa",
"doi-asserted-by": "crossref",
"first-page": "1287",
"issue": "16",
"journal-title": "Prostate",
"key": "10.1016/j.biopha.2023.114892_bib34",
"volume": "81",
"year": "2021"
},
{
"DOI": "10.12938/bmfh.2020-046",
"article-title": "Correlation of gut Firmicutes/Bacteroidetes ratio with fibrosis and steatosis stratified by body mass index in patients with non-alcoholic fatty liver disease",
"author": "Jasirwan",
"doi-asserted-by": "crossref",
"first-page": "50",
"issue": "1",
"journal-title": "Biosci. Micro, Food Health",
"key": "10.1016/j.biopha.2023.114892_bib35",
"volume": "40",
"year": "2021"
},
{
"DOI": "10.3390/jcm12062216",
"article-title": "The firmicutes/bacteroidetes ratio as a risk factor of breast cancer",
"author": "An",
"doi-asserted-by": "crossref",
"issue": "6",
"journal-title": "J. Clin. Med.",
"key": "10.1016/j.biopha.2023.114892_bib36",
"volume": "12",
"year": "2023"
},
{
"DOI": "10.3390/microorganisms8111715",
"article-title": "The influence of probiotics on the firmicutes/bacteroidetes ratio in the treatment of obesity and inflammatory bowel disease",
"author": "Stojanov",
"doi-asserted-by": "crossref",
"issue": "11",
"journal-title": "Microorganisms",
"key": "10.1016/j.biopha.2023.114892_bib37",
"volume": "8",
"year": "2020"
}
],
"reference-count": 37,
"references-count": 37,
"relation": {},
"resource": {
"primary": {
"URL": "https://linkinghub.elsevier.com/retrieve/pii/S0753332223006820"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"Pharmacology",
"General Medicine"
],
"subtitle": [],
"title": "The F/B ratio as a biomarker for inflammation in COVID-19 and T2D: Impact of metformin",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.1016/elsevier_cm_policy",
"volume": "163"
}
