Vitamin D Deficiency and Clinical Outcomes in Patients with COVID-19
et al., University of Thi-Qar Journal of Medicine, 25:1, May 2023
Vitamin D for COVID-19
8th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 135 studies, recognized in 18 countries.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
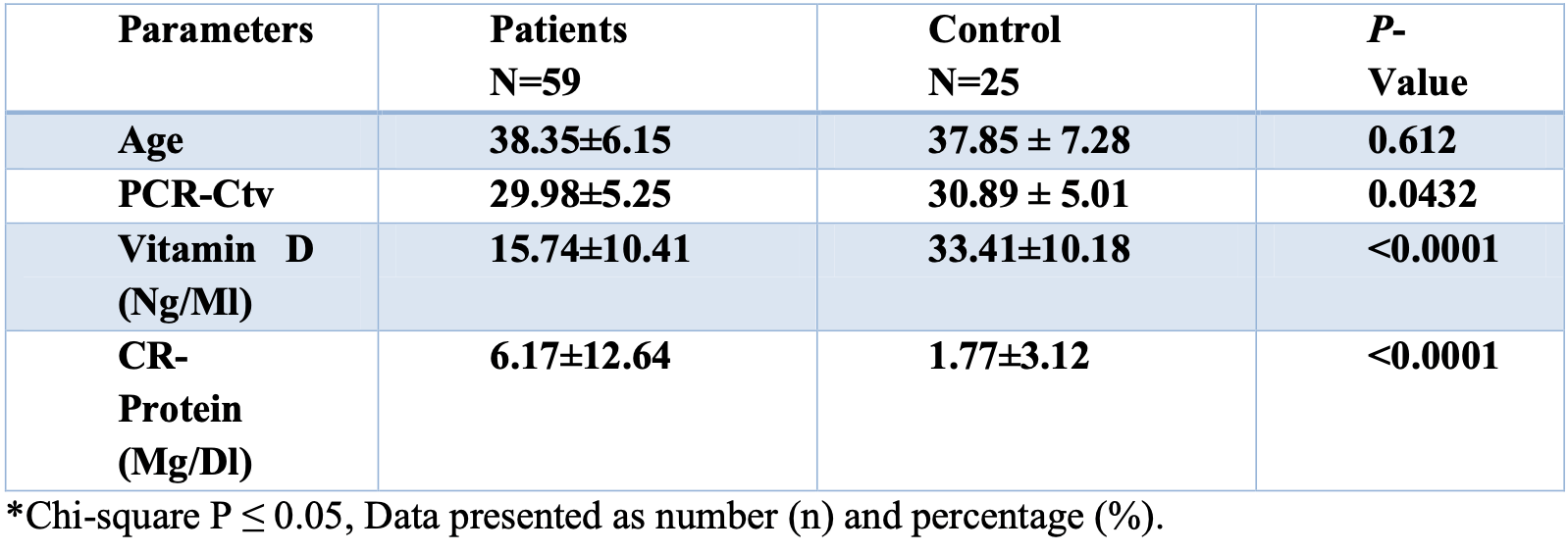
Analysis of 59 COVID-19 patients and 25 healthy controls in Iraq, showing lower vitamin D levels in COVID-19 patients.
Saeed et al., 29 May 2023, retrospective, Iraq, peer-reviewed, 6 authors.
PCR had no significantly reported differences between COVID-19 cases and control group 29.98±5.25 vs 39.89 ± 5.01.
Conclusion: we found that COVID-19 patients with vitamin D deficiency were more likely to increase the risk of severe COVID-19 infection and complications; it helps regulate the body's inflammatory response, which is important in fighting off infections.
Ethics Statement and Consent to Participate The protocol was approved by the Ethics Licensing Committee of Sulaimani Polytechnic University, Kalar Technical College (No. KTC09 on February 5, 2023) and followed the Helsinki Declaration. All participants provided written informed consent and permission for publication, and the study adhered to the ARRIVE 2.0 principles. Permission to publish was obtained by signing the approved agreement of all study participants. All techniques were consistent with the Helsinki Declaration of 1964. Questionnaire for all participants were filled for those section that are required.
References
Ahmed, Saeed, Ali, Ali, Rostam, The Impact of Smoking on COVID-19 Severity : A Multi-Analysis Study
Ali, Ali, Fatah, Tawfeeq, Rostam, SARS-CoV-2 reinfection in Thi, Qar Medical Journal
Ali, Ali, Rostam, Ali, Tawfeeq et al., Clinical laboratory parameters and comorbidities associated with severity of coronavirus disease 2019 (COVID-19) in Kurdistan Region of Iraq, Pract Lab Med
Ali, Ali, Tawfeeq, Figueredo, Rostam, Hypoalbuminemia in patients following their recovery from severe coronavirus disease, J Med Virol, doi:10.1002/jmv.27002
Ali, Rostam, Fatah, Noori, Ali et al., Serum troponin, Ddimer, and CRP level in severe coronavirus (COVID-19) patients, Immunity, Inflamm Dis, doi:10.1002/iid3.582
Ali, Tofiq, Rostam, Ali, Tawfeeq, Disease severity and efficacy of homologous vaccination among patients infected with SARS-CoV-2 Delta or Omicron VOCs, compared to unvaccinated using main biomarkers, J Med Virol, doi:10.1002/jmv.28098
Ali, Tofiq, Rostam, Ali, Th, Reply to Letter to the Editor on disease severity and efficacy of homologous vaccination among patients infected with SARS-CoV-2 Delta or Omicron VOCs, compared to unvaccinated using main biomarkers, J Med Virol, doi:10.1002/jmv.28313
Anand, Stahel, Review the safety of Covid-19 mRNA vaccines: a review, Patient Saf Surg. Patient Safety in Surgery, doi:10.1186/s13037-021-00291-9
Da, Mesquita, Silva Junior, Santana, De Oliveira et al., Clinical manifestations of COVID-19 in the general population: systematic review, Wien Klin Wochenschr, doi:10.1007/s00508-020-01760-4
Daneshkhah, Agrawal, Eshein, Subramanian, Roy et al., The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients. medRxiv [Internet], doi:10.1101/2020.04.08.20058578v4%0Ahttps://www.medrxiv.org/content/10.1101/2020.04.08.20058578v4.abstract
Eaaswarkhanth, Madhoun, Al-Mulla, Could the D614G substitution in the SARS-CoV-2 spike (S) protein be associated with higher COVID-19 mortality?, doi:10.1016/j.ijid.2020.05.071
Elibol, Baran, The relation between serum D-dimer, ferritin and vitamin D levels, and dysgeusia symptoms, in patients with coronavirus disease, J Laryngol Otol, doi:10.1017/S0022215120002765
Elsevier, None, doi:10.1016/j.plabm.2022.e00294
Fateh, Ali, Association between diet quality and BMI with side e ff ects of P fi zer-BioNTech COVID-19 vaccine and SARS-CoV-2 immunoglobulin G titers, doi:10.1108/NFS-09-2022-0338
Fotuhi, Mian, Meysami, Raji, Neurobiology of COVID-19, J Alzheimer's Dis, doi:10.3233/JAD-200581
Kim, The role of vitamin D in thyroid diseases, Int J Mol Sci, doi:10.3390/ijms18091949
Larijani, Hossein-Nezhad, Feizabad, Maghbooli, Adibi et al., Vitamin D deficiency, bone turnover markers and causative factors among adolescents: A crosssectional study, Journal of Diabetes & Metabolic Disorders, doi:10.1186/s40200-016-0266-2
Liu, Voors, Van Veldhuisen, Der Veer, Belonje et al., Vitamin D status and outcomes in heart failure patients, Eur J Heart Fail, doi:10.1093/eurjhf/hfr032
Malik, Patel, Mehta, Patel, Kelkar et al., Biomarkers and outcomes of COVID-19 hospitalisations: Systematic review and meta-analysis, BMJ Evidence-Based Med, doi:10.1136/bmjebm-2020-111536
Parlak, Ertürk, Çağ, Sebin, Gümüşdere, The effect of inflammatory cytokines and the level of vitamin D on prognosis in Crimean-Congo hemorrhagic fever, Int J Clin Exp Med
Patanavanich, Glantz, Smoking is associated with COVID-19 progression: A metaanalysis, Nicotine Tob Res, doi:10.1093/ntr/ntaa082
Serio, Lovero, Agostino, Nisi, Miragliotta et al., Evaluation of procalcitonin, Vitamin D and C-reactive protein levels in septic patients with positive emocoltures. Our preliminary experience, Acta Medica Mediterr, doi:10.19193/0393-6384_2016_6_182
Shastri, Parikh, Aggarwal, Agrawal, Chatterjee et al., Severe SARS-CoV-2 Breakthrough Reinfection With Delta Variant After Recovery From Breakthrough Infection by Alpha Variant in a Fully Vaccinated Health Worker, Front Med, doi:10.3389/fmed.2021.737007
Wruck, Adjaye, Detailed phylogenetic analysis tracks transmission of distinct SARS-COV-2 variants from China and Europe to West Africa, Nature Publishing Group UK, doi:10.1038/s41598-021-00267-w
Wuhan, China: a retrospective cohort study, Lancet, doi:10.1016/S0140-6736(20)30566-3
Xu, Song, Zhang, Fu, Gao et al., The Vitamin D status is associated with serum C-reactive protein and adhesion molecules in patients with renal cell carcinoma, Sci Rep, doi:10.1038/s41598-019-53399
Yin, Agrawal, Vitamin D and inflammatory diseases, J Inflamm Res, doi:10.2147/JIR.S63898
Zhou, Yu, Du, Fan, Liu et al., Clinical course and risk factors for mortality of adult inpatients with
