Working-from-home persistently influences sleep and physical activity 2 years after the Covid-19 pandemic onset: a longitudinal sleep tracker and electronic diary-based study
et al., Frontiers in Psychology, doi:10.3389/fpsyg.2023.1145893, May 2023
Exercise for COVID-19
9th treatment shown to reduce risk in
October 2020, now with p < 0.00000000001 from 68 studies.
No treatment is 100% effective. Protocols
combine treatments.
6,400+ studies for
210+ treatments. c19early.org
|
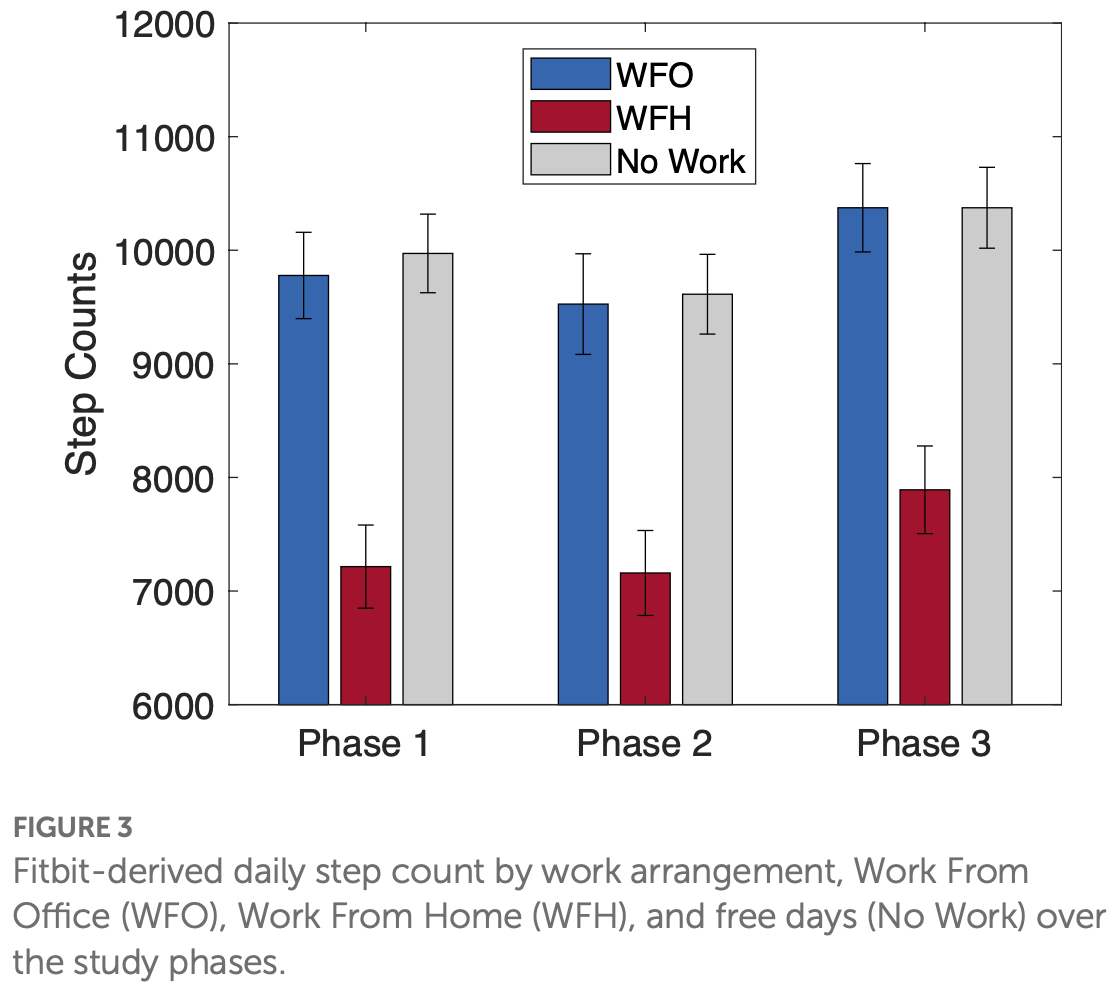
Analysis of 225 adults in Singapore showing working from home associated with lower physical activity (as measured by step count) during August 2021 - January 2022.
Massar et al., 5 May 2023, Singapore, peer-reviewed, mean age 35.5, 8 authors, study period August 2021 - January 2022.
Contact: michael.chee@nus.edu.sg.
Working-from-home persistently influences sleep and physical activity 2 years after the Covid-19 pandemic onset: a longitudinal sleep tracker and electronic diary-based study
Frontiers in Psychology, doi:10.3389/fpsyg.2023.1145893
Objective: Working from home (WFH) has become common place since the Covid-19 pandemic. Early studies observed population-level shifts in sleep patterns (later and longer sleep) and physical activity (reduced PA), during home confinement. Other studies found these changes to depend on the proportion of days that individuals WFH (vs. work from office; WFO). Here, we examined the effects of WFH on sleep and activity patterns in the transition to normality during the later stages of the Covid-19 pandemic (Aug 2021-Jan 2022). Methods: Two-hundred and twenty-five working adults enrolled in a public health study were followed for 22 weeks. Sleep and activity data were collected with a consumer fitness tracker (Fitbit Versa 2). Over three 2-week periods (Phase 1/week 1-2: August 16-29, 2021; Phase 2/week 11-12: October 25-November 7, 2021; Phase 3/week 21-22: January 3-16, 2022), participants provided daily Fitbit sleep and activity records. Additionally, they completed daily phone-based ecological momentary assessment (EMA), providing ratings of sleep quality, wellbeing (mood, stress, motivation), and information on daily work arrangements (WFH, WFO, no work). Work arrangement data were used to examine the effects of WFH vs. WFO on sleep, activity, and wellbeing.
Results: The proportion of WFH vs. WFO days fluctuated over the three measurement periods, mirroring evolving Covid restrictions. Across all three measurement periods WFH days were robustly associated with later bedtimes (+14.7 min), later wake times (+42.3 min), and longer Total Sleep Time (+20.2 min), compared to WFO days. Sleep efficiency was not affected. WFH was further associated with lower daily step count than WFO (-2,471 steps/day). WFH was associated with higher wellbeing ratings compared to WFO for those participants who had no children. However, for participants with children, these differences were not present.
Conclusion: Pandemic-initiated changes in sleep and physical activity were sustained during the later stage of the pandemic. These changes could have longer term effects, and conscious effort is encouraged to harness the benefits (i.e., longer sleep), and mitigate the pitfalls (i.e., less physical activity). These
Ethics statement This study involving human participants was reviewed and approved by The National Healthcare Group Domain Specific Review Board. The participants provided their written informed consent to participate in this study.
Author contributions SM and JO have written the manuscript and have analysed the data. TL has analyzed the data. BN, LC, DK, and KC have coordinated the study. MC has provided supervision and has reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1145893/ full#supplementary-material
References
Aili, Astrom-Paulsson, Stoetzer, Svartengren, Hillert, Reliability of Actigraphy and subjective sleep measurements in adults: the Design of Sleep Assessments, J. Clin. Sleep Med, doi:10.5664/jcsm.6384
Amicucci, Salfi, D'atri, Viselli, Ferrara, The differential impact of COVID-19 lockdown on sleep quality, insomnia, depression, stress, and anxiety among late adolescents and elderly in Italy, Brain Sci, doi:10.3390/brainsci11101336
Baazil, Cras, Dutch house approves to make work from home a legal right
Barbieri, Giuntella, Saccardo, Sadoff, Lifestyle and mental health 1 year into COVID-19, Sci. Rep, doi:10.1038/s41598-021-02702-4
Blume, Schmidt, Cajochen, Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms, Curr. Biol, doi:10.1016/j.cub.2020.06.021
Brinberg, Pincus, Conroy, The questionable ecological validity of ecological momentary assessment: considerations for design and analysis
Casagrande, Favieri, Tambelli, Forte, The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population, Sleep Med, doi:10.1016/j.sleep.2020.05.011
Cellini, Canale, Mioni, Costa, Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy, J. Sleep Res, doi:10.1111/jsr.13074
Cellini, Conte, De Rosa, Giganti, Malloggi et al., Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors, Sleep Med, doi:10.1016/j.sleep.2020.11.027
Chirico, Zaffina, Di Prinzio, Giorgi, Ferrari et al., Working from home in the context of COVID-19: a systematic review of physical and mental health effects on teleworkers, J. Health Soc. Sci, doi:10.19204/2021/wrkn8
Conroy, Hadler, Cho, Moreira, Mac Kenzie et al., The effects of COVID-19 stay-at-home order on sleep, health, and working patterns: a survey study of US health care workers, J. Clin. Sleep Med, doi:10.5664/jcsm.8808
Franceschini, Musetti, Zenesini, Palagini, Scarpelli et al., Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy, Front. Psychol, doi:10.3389/fpsyg.2020.574475
Gilson, Coenen, Hallman, Holtermann, Mathiassen et al., Postpandemic hybrid work: opportunities and challenges for physical activity and public health, Br. J. Sports Med, doi:10.1136/bjsports-2022-105664
Giuntella, Hyde, Saccardo, Sadoff, Lifestyle and mental health disruptions during COVID-19, Proc. Natl. Acad. Sci. U. S. A, doi:10.1073/pnas.2016632118
Hallman, Januario, Mathiassen, Heiden, Svensson et al., Working from home during the COVID-19 outbreak in Sweden: effects on 24-h time-use in office workers, BMC Public Health, doi:10.1186/s12889-021-10582-6
Hillman, Mitchell, Streatfeild, Burns, Bruck et al., The economic cost of inadequate sleep, Sleep, doi:10.1093/sleep/zsy083
Kniffin, Narayanan, Anseel, Antonakis, Ashford et al., COVID-19 and the workplace: implications, issues, and insights for future research and action, Am. Psychol, doi:10.1037/amp0000716
Korman, Tkachev, Reis, Komada, Kitamura et al., None
Lau, Ong, Ng, Chan, Koek et al., Minimum number of nights for reliable estimation of habitual sleep using a consumer sleep tracker, SLEEP Adv, doi:10.1093/sleepadvances/zpac026
Leone, Sigman, Golombek, Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic, Curr. Biol, doi:10.1016/j.cub.2020.07.015
Lim, Ramamurthy, Aishworiya, Rajgor, Tran et al., School closure during the coronavirus disease 2019 (COVID-19) pandemic -impact on children's sleep, Sleep Med, doi:10.1016/j.sleep.2020.12.025
Massar, Chua, Soon, Ng, Ong et al., None
Massar, Ng, Soon, Ong, Chua et al., Reopening after lockdown: the influence of working-from-home and digital device use on sleep, physical activity, and wellbeing following COVID-19 lockdown and reopening, Sleep, doi:10.1093/sleep/zsab250
Massar, Ong, Cheer, Impact of COVID-19 Mobility Restrictions on Sleep and Well-Being, Progress in Sleep Research, doi:10.1007/978-981-99-0240-8_8
Mathews, Hou, Phoa, Morin, Carrier et al., Moving forward through COVID-19 in Singapore: Well-being, lessons learnt and future directions, Can. J. Public Health, doi:10.17269/s41997-020-00382-7
Ong, Lau, Karsikas, Kinnunen, Chee et al., A longitudinal analysis of COVID-19 lockdown stringency on sleep and resting heart rate measures across 20 countries, Sci. Rep, doi:10.1038/s41598-021-93924-z
Ong, Massar, Lau, Ng, Chan et al., None
Pepin, Bailly, Mordret, Gaucher, Tamisier et al., None
Pilcher, Morris, Sleep and organizational behavior: implications for workplace productivity and safety, Front. Psychol, doi:10.3389/fpsyg.2020.00045
Raman, Coogan, Effects of societal-level COVID-19 mitigation measures on the timing and quality of sleep in Ireland, Sleep Med, doi:10.1016/j.sleep.2021.02.024
Restrepo, Zeballos, Changes in sleep duration, timing, and variability during the COVID-19 pandemic: large-scale Fitbit data from 6 major US cities, Rev. Econ. Househ, doi:10.1016/j.sleh.2021.02.008
Robbins, Affouf, Weaver, Czeisler, Barger et al., Estimated sleep duration before and during the COVID-19 pandemic in major metropolitan areas on different continents: observational study of smartphone app data, J. Med. Internet Res, doi:10.2196/20546
Saad, Wigert, Salfi, Amicucci, Corigliano et al., Two years after lockdown: longitudinal trajectories of sleep disturbances and mental health over the COVID-19 pandemic, and the effects of age, gender and chronotype, J. Sleep Res, doi:10.1111/jsr.13767
Savage, Scarpelli, Zagaria, Ratti, Albano et al., Subjective sleep alterations in healthy subjects worldwide during COVID-19 pandemic: a systematic review, meta-analysis and meta-regression, doi:10.1016/j.sleep.2022.07.012
Senatori, Spinelli, (re-)regulating remote work in the post-pandemic scenario: lessons from the Italian experience, Ital. Labour Law e-Journal, doi:10.6092/issn.1561-8048/13376
Shirmohammadi, Chan Au, Beigi, Antecedents and outcomes of work-life balance while working from home: a review of the research conducted during the COVID-19 pandemic, Hum. Resour. Dev. Rev, doi:10.1177/15344843221125834
Tejero, Seva, Fadrilan-Camacho, Factors associated with work-life balance and productivity before and during work from home, J. Occup. Environ. Med, doi:10.1097/JOM.0000000000002377
Varma, Burge, Meaklim, Junge, Jackson, Poor sleep quality and its relationship with individual characteristics, personal experiences and mental health during the COVID-19 pandemic, Int. J. Environ. Res. Public Health, doi:10.3390/ijerph18116030
Vieira, Potrich, Bressan, Klein, Loss of financial well-being in the COVID-19 pandemic: does job stability make a difference?, J. Behav. Exp. Finan, doi:10.1016/j.jbef.2021.100554
Wingard, Elon Musk's big bet against remote work: Will tesla win?
Wright, Linton, Withrow, Casiraghi, Lanza et al., Sleep in university students prior to and during COVID-19 stay-at-home orders, Curr. Biol, doi:10.1016/j.cub.2020.06.022
Wrzus, Neubauer, Ecological momentary assessment: a Metaanalysis on designs, samples, and compliance across research fields, doi:10.1177/10731911211067538
DOI record:
{
"DOI": "10.3389/fpsyg.2023.1145893",
"ISSN": [
"1664-1078"
],
"URL": "http://dx.doi.org/10.3389/fpsyg.2023.1145893",
"abstract": "<jats:sec><jats:title>Objective</jats:title><jats:p>Working from home (WFH) has become common place since the Covid-19 pandemic. Early studies observed population-level shifts in sleep patterns (later and longer sleep) and physical activity (reduced PA), during home confinement. Other studies found these changes to depend on the proportion of days that individuals WFH (vs. work from office; WFO). Here, we examined the effects of WFH on sleep and activity patterns in the transition to normality during the later stages of the Covid-19 pandemic (Aug 2021–Jan 2022).</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>Two-hundred and twenty-five working adults enrolled in a public health study were followed for 22 weeks. Sleep and activity data were collected with a consumer fitness tracker (Fitbit Versa 2). Over three 2-week periods (Phase 1/week 1–2: August 16–29, 2021; Phase 2/week 11–12: October 25–November 7, 2021; Phase 3/week 21–22: January 3–16, 2022), participants provided daily Fitbit sleep and activity records. Additionally, they completed daily phone-based ecological momentary assessment (EMA), providing ratings of sleep quality, wellbeing (mood, stress, motivation), and information on daily work arrangements (WFH, WFO, no work). Work arrangement data were used to examine the effects of WFH vs. WFO on sleep, activity, and wellbeing.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>The proportion of WFH vs. WFO days fluctuated over the three measurement periods, mirroring evolving Covid restrictions. Across all three measurement periods WFH days were robustly associated with later bedtimes (+14.7 min), later wake times (+42.3 min), and longer Total Sleep Time (+20.2 min), compared to WFO days. Sleep efficiency was not affected. WFH was further associated with lower daily step count than WFO (−2,471 steps/day). WFH was associated with higher wellbeing ratings compared to WFO for those participants who had no children. However, for participants with children, these differences were not present.</jats:p></jats:sec><jats:sec><jats:title>Conclusion</jats:title><jats:p>Pandemic-initiated changes in sleep and physical activity were sustained during the later stage of the pandemic. These changes could have longer term effects, and conscious effort is encouraged to harness the benefits (i.e., longer sleep), and mitigate the pitfalls (i.e., less physical activity). These findings are relevant for public health as hybrid WHF is likely to persist in a post-pandemic world.</jats:p></jats:sec>",
"alternative-id": [
"10.3389/fpsyg.2023.1145893"
],
"author": [
{
"affiliation": [],
"family": "Massar",
"given": "Stijn A. A.",
"sequence": "first"
},
{
"affiliation": [],
"family": "Ong",
"given": "Ju Lynn",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Lau",
"given": "TeYang",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Ng",
"given": "Ben K. L.",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chan",
"given": "Lit Fai",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Koek",
"given": "Daphne",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Cheong",
"given": "Karen",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Chee",
"given": "Michael W. L.",
"sequence": "additional"
}
],
"container-title": "Frontiers in Psychology",
"container-title-short": "Front. Psychol.",
"content-domain": {
"crossmark-restriction": true,
"domain": [
"frontiersin.org"
]
},
"created": {
"date-parts": [
[
2023,
5,
5
]
],
"date-time": "2023-05-05T06:12:16Z",
"timestamp": 1683267136000
},
"deposited": {
"date-parts": [
[
2023,
5,
5
]
],
"date-time": "2023-05-05T06:12:24Z",
"timestamp": 1683267144000
},
"indexed": {
"date-parts": [
[
2023,
5,
6
]
],
"date-time": "2023-05-06T04:30:51Z",
"timestamp": 1683347451585
},
"is-referenced-by-count": 0,
"issued": {
"date-parts": [
[
2023,
5,
5
]
]
},
"license": [
{
"URL": "https://creativecommons.org/licenses/by/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2023,
5,
5
]
],
"date-time": "2023-05-05T00:00:00Z",
"timestamp": 1683244800000
}
}
],
"link": [
{
"URL": "https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1145893/full",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "1965",
"original-title": [],
"prefix": "10.3389",
"published": {
"date-parts": [
[
2023,
5,
5
]
]
},
"published-online": {
"date-parts": [
[
2023,
5,
5
]
]
},
"publisher": "Frontiers Media SA",
"reference": [
{
"DOI": "10.5664/jcsm.6384",
"article-title": "Reliability of Actigraphy and subjective sleep measurements in adults: the Design of Sleep Assessments",
"author": "Aili",
"doi-asserted-by": "publisher",
"first-page": "39",
"journal-title": "J. Clin. Sleep Med.",
"key": "ref1",
"volume": "13",
"year": "2017"
},
{
"DOI": "10.3390/brainsci11101336",
"article-title": "The differential impact of COVID-19 lockdown on sleep quality, insomnia, depression, stress, and anxiety among late adolescents and elderly in Italy",
"author": "Amicucci",
"doi-asserted-by": "publisher",
"first-page": "1336",
"journal-title": "Brain Sci.",
"key": "ref2",
"volume": "11",
"year": "2021"
},
{
"article-title": "Dutch house approves to make work from home a legal right",
"author": "Baazil",
"key": "ref3",
"year": "2022"
},
{
"DOI": "10.1038/s41598-021-02702-4",
"article-title": "Lifestyle and mental health 1 year into COVID-19",
"author": "Barbieri",
"doi-asserted-by": "publisher",
"first-page": "23349",
"journal-title": "Sci. Rep.",
"key": "ref4",
"volume": "11",
"year": "2021"
},
{
"DOI": "10.1016/j.cub.2020.06.021",
"article-title": "Effects of the COVID-19 lockdown on human sleep and rest-activity rhythms",
"author": "Blume",
"doi-asserted-by": "publisher",
"first-page": "R795",
"journal-title": "Curr. Biol.",
"key": "ref5",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1016/j.sleep.2020.05.011",
"article-title": "The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population",
"author": "Casagrande",
"doi-asserted-by": "publisher",
"first-page": "12",
"journal-title": "Sleep Med.",
"key": "ref6",
"volume": "75",
"year": "2020"
},
{
"DOI": "10.1111/jsr.13074",
"article-title": "Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy",
"author": "Cellini",
"doi-asserted-by": "publisher",
"first-page": "e13074",
"journal-title": "J. Sleep Res.",
"key": "ref7",
"volume": "29",
"year": "2020"
},
{
"DOI": "10.1016/j.sleep.2020.11.027",
"article-title": "Changes in sleep timing and subjective sleep quality during the COVID-19 lockdown in Italy and Belgium: age, gender and working status as modulating factors",
"author": "Cellini",
"doi-asserted-by": "publisher",
"first-page": "112",
"journal-title": "Sleep Med.",
"key": "ref8",
"volume": "77",
"year": "2021"
},
{
"DOI": "10.19204/2021/wrkn8",
"article-title": "Working from home in the context of COVID-19: a systematic review of physical and mental health effects on teleworkers",
"author": "Chirico",
"doi-asserted-by": "publisher",
"first-page": "319",
"journal-title": "J. Health Soc. Sci.",
"key": "ref9",
"volume": "6",
"year": "2021"
},
{
"DOI": "10.5664/jcsm.8808",
"article-title": "The effects of COVID-19 stay-at-home order on sleep, health, and working patterns: a survey study of US health care workers",
"author": "Conroy",
"doi-asserted-by": "publisher",
"first-page": "185",
"journal-title": "J. Clin. Sleep Med.",
"key": "ref10",
"volume": "17",
"year": "2021"
},
{
"DOI": "10.3389/fpsyg.2020.574475",
"article-title": "Poor sleep quality and its consequences on mental health during the COVID-19 lockdown in Italy",
"author": "Franceschini",
"doi-asserted-by": "publisher",
"first-page": "574475",
"journal-title": "Front. Psychol.",
"key": "ref11",
"volume": "11",
"year": "2020"
},
{
"DOI": "10.1136/bjsports-2022-105664",
"article-title": "Postpandemic hybrid work: opportunities and challenges for physical activity and public health",
"author": "Gilson",
"doi-asserted-by": "publisher",
"first-page": "1203",
"journal-title": "Br. J. Sports Med.",
"key": "ref12",
"volume": "56",
"year": "2022"
},
{
"DOI": "10.1073/pnas.2016632118",
"article-title": "Lifestyle and mental health disruptions during COVID-19",
"author": "Giuntella",
"doi-asserted-by": "publisher",
"first-page": "e2016632118",
"journal-title": "Proc. Natl. Acad. Sci. U. S. A.",
"key": "ref13",
"volume": "118",
"year": "2021"
},
{
"DOI": "10.1186/s12889-021-10582-6",
"article-title": "Working from home during the COVID-19 outbreak in Sweden: effects on 24-h time-use in office workers",
"author": "Hallman",
"doi-asserted-by": "publisher",
"first-page": "528",
"journal-title": "BMC Public Health",
"key": "ref14",
"volume": "21",
"year": "2021"
},
{
"DOI": "10.1093/sleep/zsy083",
"article-title": "The economic cost of inadequate sleep",
"author": "Hillman",
"doi-asserted-by": "publisher",
"journal-title": "Sleep",
"key": "ref15",
"volume": "41",
"year": "2018"
},
{
"DOI": "10.1037/amp0000716",
"article-title": "COVID-19 and the workplace: implications, issues, and insights for future research and action",
"author": "Kniffin",
"doi-asserted-by": "publisher",
"first-page": "63",
"journal-title": "Am. Psychol.",
"key": "ref16",
"volume": "76",
"year": "2021"
},
{
"DOI": "10.1038/s41598-020-79299-7",
"article-title": "COVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock",
"author": "Korman",
"doi-asserted-by": "publisher",
"first-page": "22225",
"journal-title": "Sci. Rep.",
"key": "ref17",
"volume": "10",
"year": "2020"
},
{
"DOI": "10.1093/sleepadvances/zpac026",
"article-title": "Minimum number of nights for reliable estimation of habitual sleep using a consumer sleep tracker",
"author": "Lau",
"doi-asserted-by": "publisher",
"first-page": "zpac026",
"journal-title": "SLEEP Adv.",
"key": "ref18",
"volume": "3",
"year": "2022"
},
{
"DOI": "10.1016/j.cub.2020.07.015",
"article-title": "Effects of lockdown on human sleep and chronotype during the COVID-19 pandemic",
"author": "Leone",
"doi-asserted-by": "publisher",
"first-page": "R930",
"journal-title": "Curr. Biol.",
"key": "ref19",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1016/j.sleep.2020.12.025",
"article-title": "School closure during the coronavirus disease 2019 (COVID-19) pandemic - impact on children's sleep",
"author": "Lim",
"doi-asserted-by": "publisher",
"first-page": "108",
"journal-title": "Sleep Med.",
"key": "ref20",
"volume": "78",
"year": "2021"
},
{
"DOI": "10.1038/s41746-021-00466-9",
"article-title": "Trait-like nocturnal sleep behavior identified by combining wearable, phone-use, and self-report data",
"author": "Massar",
"doi-asserted-by": "publisher",
"first-page": "90",
"journal-title": "NPJ Digit. Med.",
"key": "ref21",
"volume": "4",
"year": "2021"
},
{
"DOI": "10.1093/sleep/zsab250",
"article-title": "Reopening after lockdown: the influence of working-from-home and digital device use on sleep, physical activity, and wellbeing following COVID-19 lockdown and reopening",
"author": "Massar",
"doi-asserted-by": "publisher",
"first-page": "zsab250",
"journal-title": "Sleep",
"key": "ref22",
"volume": "45",
"year": "2022"
},
{
"DOI": "10.1007/978-981-99-0240-8_8",
"article-title": "Impact of COVID-19 Mobility Restrictions on Sleep and Well-Being",
"author": "Massar",
"doi-asserted-by": "publisher",
"journal-title": "BaHammam, A., Pandi-Perumal, S.R., Jahrami, H. (eds) COVID-19 and Sleep: A Global Outlook. Progress in Sleep Research. Springer, Singapore",
"key": "ref70",
"year": "2023"
},
{
"author": "Mathews",
"key": "ref23",
"volume-title": "Moving forward through COVID-19 in Singapore: Well-being, lessons learnt and future directions",
"year": "2022"
},
{
"DOI": "10.17269/s41997-020-00382-7",
"article-title": "Sleep and circadian rhythm in response to the COVID-19 pandemic",
"author": "Morin",
"doi-asserted-by": "publisher",
"first-page": "654",
"journal-title": "Can. J. Public Health",
"key": "ref24",
"volume": "111",
"year": "2020"
},
{
"DOI": "10.1038/s41598-021-93924-z",
"article-title": "A longitudinal analysis of COVID-19 lockdown stringency on sleep and resting heart rate measures across 20 countries",
"author": "Ong",
"doi-asserted-by": "publisher",
"first-page": "14413",
"journal-title": "Sci. Rep.",
"key": "ref25",
"volume": "11",
"year": ""
},
{
"DOI": "10.1093/sleep/zsaa179",
"article-title": "COVID-19-related mobility reduction: heterogenous effects on sleep and physical activity rhythms",
"author": "Ong",
"doi-asserted-by": "publisher",
"first-page": "zsaa179",
"journal-title": "Sleep",
"key": "ref26",
"volume": "44",
"year": ""
},
{
"DOI": "10.1093/sleep/zsac315",
"article-title": "A randomised controlled trial of a digital, small incentive-based intervention for working adults with short sleep",
"author": "Ong",
"doi-asserted-by": "publisher",
"journal-title": "Sleep",
"key": "ref27",
"year": "2022"
},
{
"DOI": "10.1093/sleep/zsab075",
"article-title": "Greatest changes in objective sleep architecture during COVID-19 lockdown in night owls with increased REM sleep",
"author": "Pepin",
"doi-asserted-by": "publisher",
"first-page": "zsab075",
"journal-title": "Sleep",
"key": "ref28",
"volume": "44",
"year": "2021"
},
{
"DOI": "10.3389/fpsyg.2020.00045",
"article-title": "Sleep and organizational behavior: implications for workplace productivity and safety",
"author": "Pilcher",
"doi-asserted-by": "publisher",
"first-page": "45",
"journal-title": "Front. Psychol.",
"key": "ref29",
"volume": "11",
"year": "2020"
},
{
"key": "ref300",
"year": "2018"
},
{
"DOI": "10.1080/15427609.2017.1340052",
"article-title": "The questionable ecological validity of ecological momentary assessment: considerations for design and analysis",
"author": "Ram",
"doi-asserted-by": "publisher",
"first-page": "253",
"journal-title": "Res. Hum. Dev.",
"key": "ref30",
"volume": "14",
"year": "2017"
},
{
"DOI": "10.1016/j.sleep.2021.02.024",
"article-title": "Effects of societal-level COVID-19 mitigation measures on the timing and quality of sleep in Ireland",
"author": "Raman",
"doi-asserted-by": "publisher",
"first-page": "179",
"journal-title": "Sleep Med.",
"key": "ref31",
"volume": "91",
"year": "2022"
},
{
"DOI": "10.1007/s11150-022-09614-w",
"article-title": "Work from home and daily time allocations: evidence from the coronavirus pandemic",
"author": "Restrepo",
"doi-asserted-by": "publisher",
"first-page": "735",
"journal-title": "Rev. Econ. Househ.",
"key": "ref32",
"volume": "20",
"year": "2022"
},
{
"DOI": "10.1016/j.sleh.2021.02.008",
"article-title": "Changes in sleep duration, timing, and variability during the COVID-19 pandemic: large-scale Fitbit data from 6 major US cities",
"author": "Rezaei",
"doi-asserted-by": "publisher",
"first-page": "303",
"journal-title": "Sleep Health",
"key": "ref33",
"volume": "7",
"year": "2021"
},
{
"DOI": "10.2196/20546",
"article-title": "Estimated sleep duration before and during the COVID-19 pandemic in major metropolitan areas on different continents: observational study of smartphone app data",
"author": "Robbins",
"doi-asserted-by": "publisher",
"first-page": "e20546",
"journal-title": "J. Med. Internet Res.",
"key": "ref34",
"volume": "23",
"year": "2021"
},
{
"author": "Saad",
"key": "ref35",
"volume-title": "Remote work persisting and trending permanent",
"year": "2021"
},
{
"DOI": "10.1111/jsr.13767",
"article-title": "Two years after lockdown: longitudinal trajectories of sleep disturbances and mental health over the COVID-19 pandemic, and the effects of age, gender and chronotype",
"author": "Salfi",
"doi-asserted-by": "publisher",
"first-page": "e13767",
"journal-title": "J. Sleep Res.",
"key": "ref36",
"year": "2022"
},
{
"author": "Savage",
"key": "ref37",
"volume-title": "What bosses really think about remote work",
"year": "2021"
},
{
"DOI": "10.1016/j.sleep.2022.07.012",
"article-title": "Subjective sleep alterations in healthy subjects worldwide during COVID-19 pandemic: a systematic review, meta-analysis and meta-regression",
"author": "Scarpelli",
"doi-asserted-by": "publisher",
"first-page": "89",
"journal-title": "Sleep Med.",
"key": "ref38",
"volume": "100",
"year": "2022"
},
{
"DOI": "10.6092/issn.1561-8048/13376",
"article-title": "(re-)regulating remote work in the post-pandemic scenario: lessons from the Italian experience",
"author": "Senatori",
"doi-asserted-by": "publisher",
"first-page": "209",
"journal-title": "Ital. Labour Law e-Journal",
"key": "ref39",
"volume": "14",
"year": "2021"
},
{
"DOI": "10.1177/15344843221125834",
"article-title": "Antecedents and outcomes of work-life balance while working from home: a review of the research conducted during the COVID-19 pandemic",
"author": "Shirmohammadi",
"doi-asserted-by": "publisher",
"first-page": "473",
"journal-title": "Hum. Resour. Dev. Rev.",
"key": "ref40",
"volume": "21",
"year": "2022"
},
{
"DOI": "10.1097/JOM.0000000000002377",
"article-title": "Factors associated with work-life balance and productivity before and during work from home",
"author": "Tejero",
"doi-asserted-by": "publisher",
"first-page": "1065",
"journal-title": "J. Occup. Environ. Med.",
"key": "ref41",
"volume": "63",
"year": "2021"
},
{
"DOI": "10.3390/ijerph18116030",
"article-title": "Poor sleep quality and its relationship with individual characteristics, personal experiences and mental health during the COVID-19 pandemic",
"author": "Varma",
"doi-asserted-by": "publisher",
"first-page": "6030",
"journal-title": "Int. J. Environ. Res. Public Health",
"key": "ref42",
"volume": "18",
"year": "2021"
},
{
"DOI": "10.1016/j.jbef.2021.100554",
"article-title": "Loss of financial well-being in the COVID-19 pandemic: does job stability make a difference?",
"author": "Vieira",
"doi-asserted-by": "publisher",
"first-page": "100554",
"journal-title": "J. Behav. Exp. Finan.",
"key": "ref43",
"volume": "31",
"year": "2021"
},
{
"author": "Wingard",
"key": "ref44",
"volume-title": "Elon Musk’s big bet against remote work: Will tesla win?",
"year": "2022"
},
{
"DOI": "10.1016/j.cub.2020.06.022",
"article-title": "Sleep in university students prior to and during COVID-19 stay-at-home orders",
"author": "Wright",
"doi-asserted-by": "publisher",
"first-page": "R797",
"journal-title": "Curr. Biol.",
"key": "ref45",
"volume": "30",
"year": "2020"
},
{
"DOI": "10.1177/10731911211067538",
"article-title": "Ecological momentary assessment: a Meta-analysis on designs, samples, and compliance across research fields",
"author": "Wrzus",
"doi-asserted-by": "publisher",
"first-page": "825",
"journal-title": "Assessment",
"key": "ref46",
"volume": "30",
"year": "2023"
}
],
"reference-count": 48,
"references-count": 48,
"relation": {},
"resource": {
"primary": {
"URL": "https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1145893/full"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [
"General Psychology"
],
"subtitle": [],
"title": "Working-from-home persistently influences sleep and physical activity 2 years after the Covid-19 pandemic onset: a longitudinal sleep tracker and electronic diary-based study",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.3389/crossmark-policy",
"volume": "14"
}
