Proton Pump Inhibitors Use and Increased Risk of Spontaneous Bacterial Peritonitis in Cirrhotic Patients: A Retrospective Cohort Analysis
et al., Gastroenterology Research, doi:10.14740/gr1545, Aug 2022
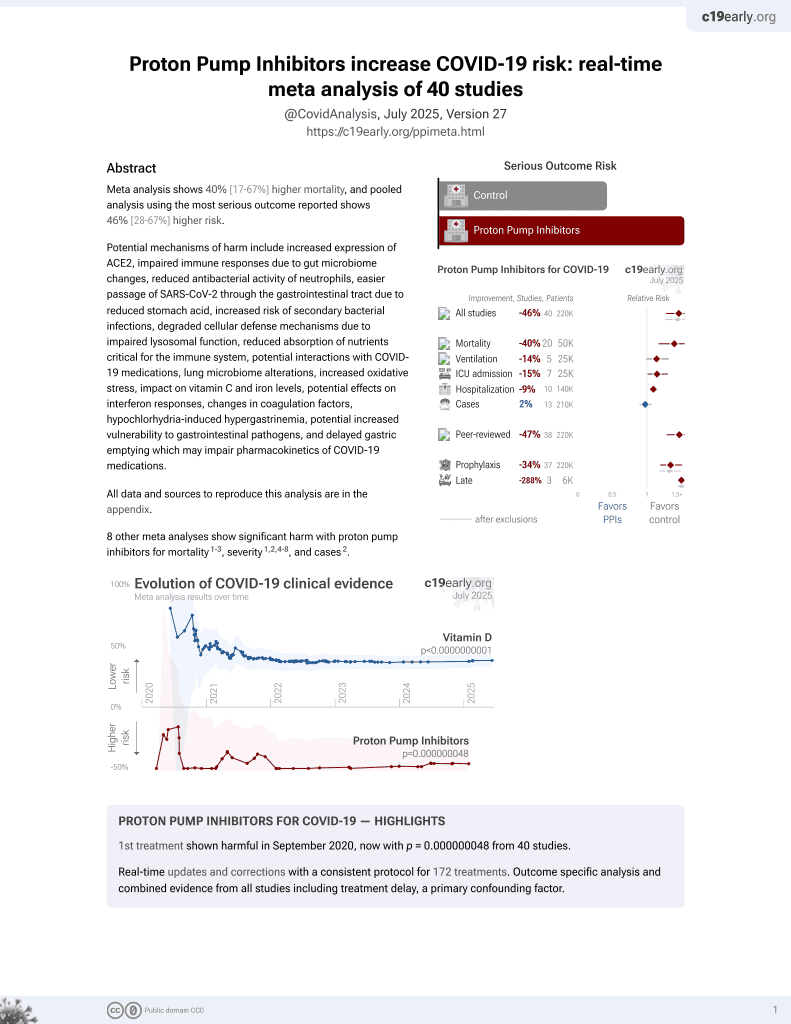
PPIs for COVID-19
1st treatment shown to increase risk in
September 2020, now with p = 0.000000048 from 40 studies.
6,400+ studies for
210+ treatments. c19early.org
|
Retrospective 107,750 cirrhotic patients showing increased risk of spontaneous bacterial peritonitis (SBP) with proton pump inhibitor (PPI) use. PPI use was the strongest predictor of SBP, with patients on PPIs 4.24 times more likely to develop SBP compared to those not on PPIs. The authors hypothesize PPIs may increase SBP risk by facilitating intestinal bacterial proliferation, impairing gastrointestinal motility and permeability, and compromising immunity in cirrhotic patients.
Dahabra et al., 31 Aug 2022, retrospective, USA, peer-reviewed, 5 authors.
Contact: ldeeb1@northwell.edu.
Proton Pump Inhibitors Use and Increased Risk of Spontaneous Bacterial Peritonitis in Cirrhotic Patients: A Retrospective Cohort Analysis
Gastroenterology Research, doi:10.14740/gr1545
Background: Since their introduction in the early 1980s, proton pump inhibitors (PPIs) have been used worldwide for a broad range of indications. Unfortunately, however, PPIs have become overly prescribed by healthcare providers, sometimes in the absence of clear indications. Although PPIs were initially presumed to have an excellent safety profile, emerging studies have shed light on the association between their long-term use and a myriad of side effects, including the possibility of an increased risk of spontaneous bacterial peritonitis (SBP). Data available to date regarding the association between PPI use and SBP development in cirrhotic patients is conflicting. While some observational studies provide no association between PPI use in cirrhotic patients and an increased risk of SBP development, many others support this association. As a result of the conflicting conclusions from case controls, cohorts, and meta-analyses, we aimed to carry out this retrospective cohort analysis of data from cirrhotic patients included in the electronic medical record-based commercial database, EXPLORYS (IMB-WATSON, Cleveland, Ohio). Our aim was to evaluate for a possible association between PPIs use and the risk of SBP development in cirrhotic patients and to compare the prevalence of SBP development between cirrhotic patients who were actively using PPIs and those who were not.
Methods: A retrospective cohort analysis with chart review was conducted on patients with cirrhosis who were included in the electronic medical record-based commercial database, EXPLORYS (IMB-WATSON, Cleveland, Ohio). Using this database, records were reviewed between December 2017 and 2020. Included patients were adults aged 30 to 79 years with a Systematized Nomenclature of Medicine-Clinical Terms (SNOMED-CT) diagnosis of liver cirrhosis. Included patients with a SNOMED-CT diagnosis of liver cirrhosis were divided into two groups: the first group included all cirrhotic patients who did not use PPIs and the second group included all cirrhotic patients who were on PPIs at home.
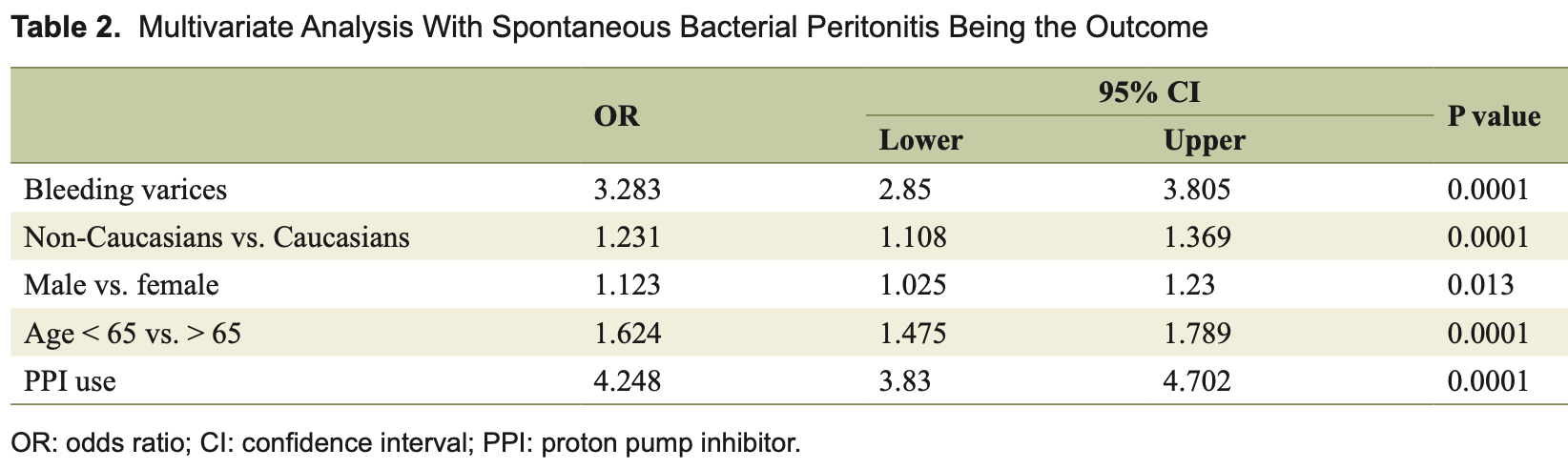
Results: In our analysis, SBP occurred in 1.7% (1,860 patients) of the included cirrhotic patients whether they were actively taking PPIs or not. Among the 40,670 cirrhotic patients who were on PPIs at home, 1,350 (3.3%) patients developed SBP. On multivariate analysis, PPI use was the strongest predictor for SBP in cirrhotic patients (odds ratio (OR) = 4.24; 95% confidence interval (CI): 3.83 -4.7, P value < 0.0001), with cirrhotic patients taking PPIs being 4.24 more likely to develop SBP than those not on PPIs. In addition, PPI use, history of bleeding varices, age, race, and gender were found to be independent predicting factors for SBP, in descending order of importance.
Conclusions: Our retrospective cohort analysis has shown that the use of PPIs in patients with liver cirrhosis is an independent predicting risk factor for SBP development. It solidified the argument that cirrhotic patients..
Financial Disclosure The authors declare no grants or financial support for the research, authorship, and publication of this article.
Conflict of Interest The authors declare that they have no competing interests.
Author Contributions LD, MA, and AAY carried out the study design, data entry, and statistical analysis. MK and LD carried out the drafting of the manuscript and its critical revision.
Abbreviations CI: confidence interval; GERD: gastroesophageal reflux disease; HLA: human leukocyte antigen; H2RA: histamine-2 receptor antagonist; ICD: International Classification of Diseases; MELD-Na: model for end-stage liver disease sodium; NSAID: non-steroidal anti-inflammatory drug; PMN: polymorphonuclear leukocyte; PPIs: proton pump inhibitors; PUD: peptic ulcer disease; RCTs: randomized clinical trials; SBP: spontaneous bacterial peritonitis; SIBO: small intestinal bacterial overgrowth; SNOMED-CT: Systematized Nomenclature of Medicine-Clinical Terms; SPSS: Statistical Package for Social Sciences
References
Agastya, West, Callahan, Omeprazole inhibits phagocytosis and acidification of phagolysosomes of normal human neutrophils in vitro, Immunopharmacol Immunotoxicol
Alhumaid, Mutair, Alawi, Zaidi, Rabaan et al., Proton pump inhibitors use and risk of developing spontaneous bacterial peritonitis in cirrhotic patients: A systematic review and meta-analysis, Gut Pathog
Bajaj, Zadvornova, Heuman, Hafeezullah, Hoffmann et al., Association of proton pump inhibitor therapy with spontaneous bacterial peritonitis in cirrhotic patients with ascites, Am J Gastroenterol
Barletta, Sclar, Proton pump inhibitors increase the risk for hospital-acquired Clostridium difficile infec-Proton Pump Inhibitors Use in Cirrhosis, Gastroenterol Res
Campbell, Obstein, Reddy, Yang, Association between proton pump inhibitor use and spontaneous bacterial peritonitis, Dig Dis Sci
Chang, Lai, Lee, Lee, Tsai et al., Risk of spontaneous bacterial peritonitis associated with gastric Acid suppression, Medicine
Dam, Vilstrup, Watson, Jepsen, Proton pump inhibitors as a risk factor for hepatic encephalopathy and spontaneous bacterial peritonitis in patients with cirrhosis with ascites, Hepatology
De Vos, Vroey, Garcia, Roy, Kidd et al., Role of proton pump inhibitors in the occurrence and the prognosis of spontaneous bacterial peritonitis in cirrhotic patients with ascites, Liver Int
Deshpande, Pasupuleti, Thota, Pant, Mapara et al., Acid-suppressive therapy is associated with spontaneous bacterial peritonitis in cirrhotic patients: a meta-analysis, J Gastroenterol Hepatol
Durand, Willett, Desilets, Proton Pump Inhibitor use in Hospitalized Patients: Is Overutilization Becoming a Problem?, Clin Med Insights Gastroenterol
Fernandez, Navasa, Gomez, Colmenero, Vila et al., Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophylaxis, Hepatology
Garcia-Martinez, Andreola, Mehta, Poulton, Oria et al., Immunomodulatory and antioxidant function of albumin stabilises the endothelium and improves survival in a rodent model of chronic liver failure, J Hepatol
Garcia-Martinez, Frances, Zapater, Gimenez, Gomez-Hurtado et al., Use of proton pump inhibitors decrease cellular oxidative burst in patients with decompensated cirrhosis, J Gastroenterol Hepatol
Garcia-Tsao, Sanyal, Grace, Practice Guidelines Committee of the American Association for the Study of Liver Diseases, Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis, Hepatology
Goel, Deshpande, Lopez, Hall, Van Duin et al., Increased rate of spontaneous bacterial peritonitis among cirrhotic patients receiving pharmacologic acid suppression, Clin Gastroenterol Hepatol
Guarner, Runyon, Young, Heck, Sheikh, Intestinal bacterial overgrowth and bacterial translocation in cirrhotic rats with ascites, J Hepatol
Herzig, Howell, Ngo, Marcantonio, Acidsuppressive medication use and the risk for hospital-acquired pneumonia, JAMA
Jacobs, Adame, Attaluri, Valestin, Rao, Dysmotility and proton pump inhibitor use are independent risk factors for small intestinal bacterial and/or fungal overgrowth, Aliment Pharmacol Ther
Kalaitzakis, Bjornsson, A review of esomeprazole in the treatment of gastroesophageal reflux disease (GERD), Ther Clin Risk Manag
Khan, Kamal, Khan, Lee, Howden, Systematic review and meta-analysis of the possible association between pharmacological gastric acid suppression and spontaneous bacterial peritonitis, Eur J Gastroenterol Hepatol
Kim, Lim, Min, Lee, Min et al., -187 for recurrent spontaneous bacterial peritonitis in patients with cirrhosis, J Gastroenterol Hepatol
Kwon, Koh, Kim, Jung, Kim et al., Mortality associated with proton pump inhibitors in cirrhotic patients with spontaneous bacterial peritonitis, J Gastroenterol Hepatol
Lagadinou, Solomou, Velissaris, Theodorou, Karakatza et al., Alterations in T-lymphocyte subpopulations in patients with complicated liver cirrhosis, Diagn Microbiol Infect Dis
Lewis, Barre, Zhu, Ivey, Lim et al., Long-term proton pump inhibitor therapy and falls and fractures in elderly women: a prospective cohort study, J Bone Miner Res
Lin, Tsai, Ho, Huang, Lin et al., Endotoxemia contributes to the immune paralysis in patients with cirrhosis, J Hepatol
Linsky, Gupta, Lawler, Fonda, Hermos, Proton pump inhibitors and risk for recurrent Clostridium difficile infection, Arch Intern Med
Lodato, Azzaroli, Girolamo, Feletti, Cecinato et al., Proton pump inhibitors in cirrhosis: tradition or evidence based practice?, World J Gastroenterol
Mandorfer, Bota, Schwabl, Bucsics, Pfisterer et al., Proton pump inhibitor intake neither predisposes to spontaneous bacterial peritonitis or other infections nor increases mortality in patients with cirrhosis and ascites, PLoS One
Merli, Lucidi, Gregorio, Giannelli, Giusto et al., The chronic use of beta-blockers and proton pump inhibitors may affect the rate of bacterial infections in cirrhosis, Liver Int
Miano, Reichert, Houle, Macgregor, Kincaid et al., Nosocomial pneumonia risk and stress ulcer prophylaxis: a comparison of pantoprazole vs ranitidine in cardiothoracic surgery patients, Chest
Miozzo, John, Appel-Da-Silva, Dossin, Tovo et al., Influence of proton pump inhibitors in the development of spontaneous bacterial peritonitis, World J Hepatol
O'brien, Fullerton, Massey, Auld, Sewell et al., Immunosuppression in acutely decompensated cirrhosis is mediated by prostaglandin E2, Nat Med
O'leary, Reddy, Wong, Kamath, Patton et al., Long-term use of antibiotics and proton pump inhibitors predict development of infections in patients with cirrhosis, Clin Gastroenterol Hepatol
Pardo, Bartoli, Lorenzo-Zuniga, Planas, Vinado et al., Effect of cisapride on intestinal bacterial overgrowth and bacterial translocation in cirrhosis, Hepatology
Ratelle, Perreault, Villeneuve, Tremblay, Association between proton pump inhibitor use and spontaneous bacterial peritonitis in cirrhotic patients with ascites, Can J Gastroenterol Hepatol
Rotman, Bishop, Proton pump inhibitor use in the U.S. ambulatory setting, 2002-2009, PLoS One
Runyon, The evolution of ascitic fluid analysis in the diagnosis of spontaneous bacterial peritonitis, Am J Gastroenterol
Savarino, Dulbecco, De Bortoli, Ottonello, Savarino, The appropriate use of proton pump inhibitors (PPIs): Need for a reappraisal, Eur J Intern Med
Savarino, Marabotto, Furnari, Zingone, Zentilin et al., Latest insights into the hot question of proton pump inhibitor safety -a narrative review, Dig Liver Dis
Sipeki, Antal-Szalmas, Lakatos, Papp, Immune dysfunction in cirrhosis, World J Gastroenterol
Siple, Morey, Gutman, Weinberg, Collins, Proton pump inhibitor use and association with spontaneous bacterial peritonitis in patients with cirrhosis and ascites, Ann Pharmacother
Study, Liver, EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis, J Hepatol
Terg, Casciato, Garbe, Cartier, Stieben et al., Proton pump inhibitor therapy does not increase the incidence of spontaneous bacterial peritonitis in cirrhosis: a multicenter prospective study, J Hepatol
Thomson, Sauve, Kassam, Kamitakahara, Safety of the long-term use of proton pump inhibitors, World J Gastroenterol
Trikudanathan, Israel, Cappa, Sullivan, Association between proton pump inhibitors and spontaneous bacterial peritonitis in cirrhotic patients -a systematic review and meta-analysis, Int J Clin Pract
Van Vlerken, Huisman, Van Hoek, Renooij, De Rooij et al., Bacterial infections in cirrhosis: role of proton pump inhibitors and intestinal permeability, Eur J Clin Invest
Welage, Berardi, Evaluation of omeprazole, lansoprazole, pantoprazole, and rabeprazole in the treatment of acid-related diseases, J Am Pharm Assoc (Wash)
Xu, Wang, Li, Ye, Dong et al., Proton pump inhibitor use and risk of spontaneous bacterial peritonitis in cirrhotic patients: a systematic review and meta-analysis, Genet Mol Res
Yang, Chang, Chen, Small-intestinal bacterial overgrowth in patients with liver cirrhosis, diagnosed with glucose H2 or CH4 breath tests, Scand J Gastroenterol
Yu, Tang, Jiang, Zheng, Xiong et al., Proton pump inhibitor therapy and its association with spontaneous bacterial peritonitis incidence and mortality: A metaanalysis, Dig Liver Dis
Zedtwitz-Liebenstein, Wenisch, Patruta, Parschalk, Daxbock et al., Omeprazole treatment diminishes intra-and extracellular neutrophil reactive oxygen production and bactericidal activity, Crit Care Med
Zhu, Yu, Mancuso, Qi, Proton pump inhibitors in liver cirrhosis: a review of benefits and harms, AME Med J
DOI record:
{
"DOI": "10.14740/gr1545",
"ISSN": [
"1918-2805",
"1918-2813"
],
"URL": "http://dx.doi.org/10.14740/gr1545",
"alternative-id": [
"10.14740/gr1545"
],
"author": [
{
"affiliation": [],
"family": "Dahabra",
"given": "Loai",
"sequence": "first"
},
{
"affiliation": [],
"family": "Kreidieh",
"given": "Malek",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abureesh",
"given": "Mohammad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Abou Yassine",
"given": "Ahmad",
"sequence": "additional"
},
{
"affiliation": [],
"family": "Deeb",
"given": "Liliane",
"sequence": "additional"
}
],
"container-title": "Gastroenterology Research",
"container-title-short": "Gastroenterol Res",
"content-domain": {
"crossmark-restriction": false,
"domain": [
"www.gastrores.org"
]
},
"created": {
"date-parts": [
[
2022,
8,
23
]
],
"date-time": "2022-08-23T12:55:22Z",
"timestamp": 1661259322000
},
"deposited": {
"date-parts": [
[
2022,
8,
24
]
],
"date-time": "2022-08-24T01:51:26Z",
"timestamp": 1661305886000
},
"indexed": {
"date-parts": [
[
2024,
7,
2
]
],
"date-time": "2024-07-02T19:12:46Z",
"timestamp": 1719947566736
},
"is-referenced-by-count": 5,
"issue": "4",
"issued": {
"date-parts": [
[
2022,
8
]
]
},
"journal-issue": {
"issue": "4"
},
"language": "en",
"license": [
{
"URL": "https://creativecommons.org/licenses/by-nc/4.0/",
"content-version": "vor",
"delay-in-days": 0,
"start": {
"date-parts": [
[
2022,
8,
1
]
],
"date-time": "2022-08-01T00:00:00Z",
"timestamp": 1659312000000
}
}
],
"link": [
{
"URL": "http://www.gastrores.org/index.php/Gastrores/article/download/1545/1510",
"content-type": "unspecified",
"content-version": "vor",
"intended-application": "similarity-checking"
}
],
"member": "5784",
"original-title": [],
"page": "180-187",
"prefix": "10.14740",
"published": {
"date-parts": [
[
2022,
8
]
]
},
"published-print": {
"date-parts": [
[
2022,
8
]
]
},
"publisher": "Elmer Press, Inc.",
"reference-count": 0,
"references-count": 0,
"relation": {},
"resource": {
"primary": {
"URL": "http://www.gastrores.org/index.php/Gastrores/article/view/1545"
}
},
"score": 1,
"short-title": [],
"source": "Crossref",
"subject": [],
"subtitle": [],
"title": "Proton Pump Inhibitors Use and Increased Risk of Spontaneous Bacterial Peritonitis in Cirrhotic Patients: A Retrospective Cohort Analysis",
"type": "journal-article",
"update-policy": "http://dx.doi.org/10.14740/elmerpress-crossmark-policy",
"volume": "15"
}