Bamlanivimab/etesevimab reduced COVID-19 risk: real-time meta analysis of 22 studies
, Dec 2025
25th treatment shown to reduce risk in
May 2021, now with p = 0.00049 from 22 studies, recognized in 11 countries.
Efficacy is variant dependent.
No treatment is 100% effective. Protocols
combine treatments.
6,300+ studies for
210+ treatments. c19early.org
|
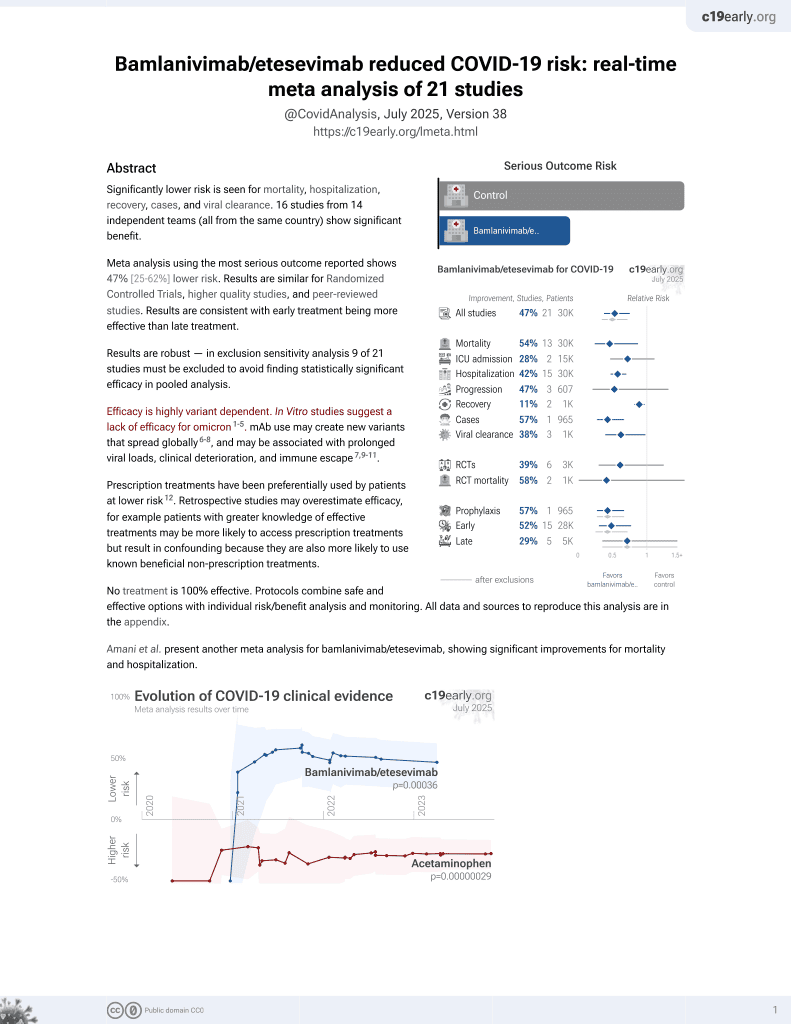
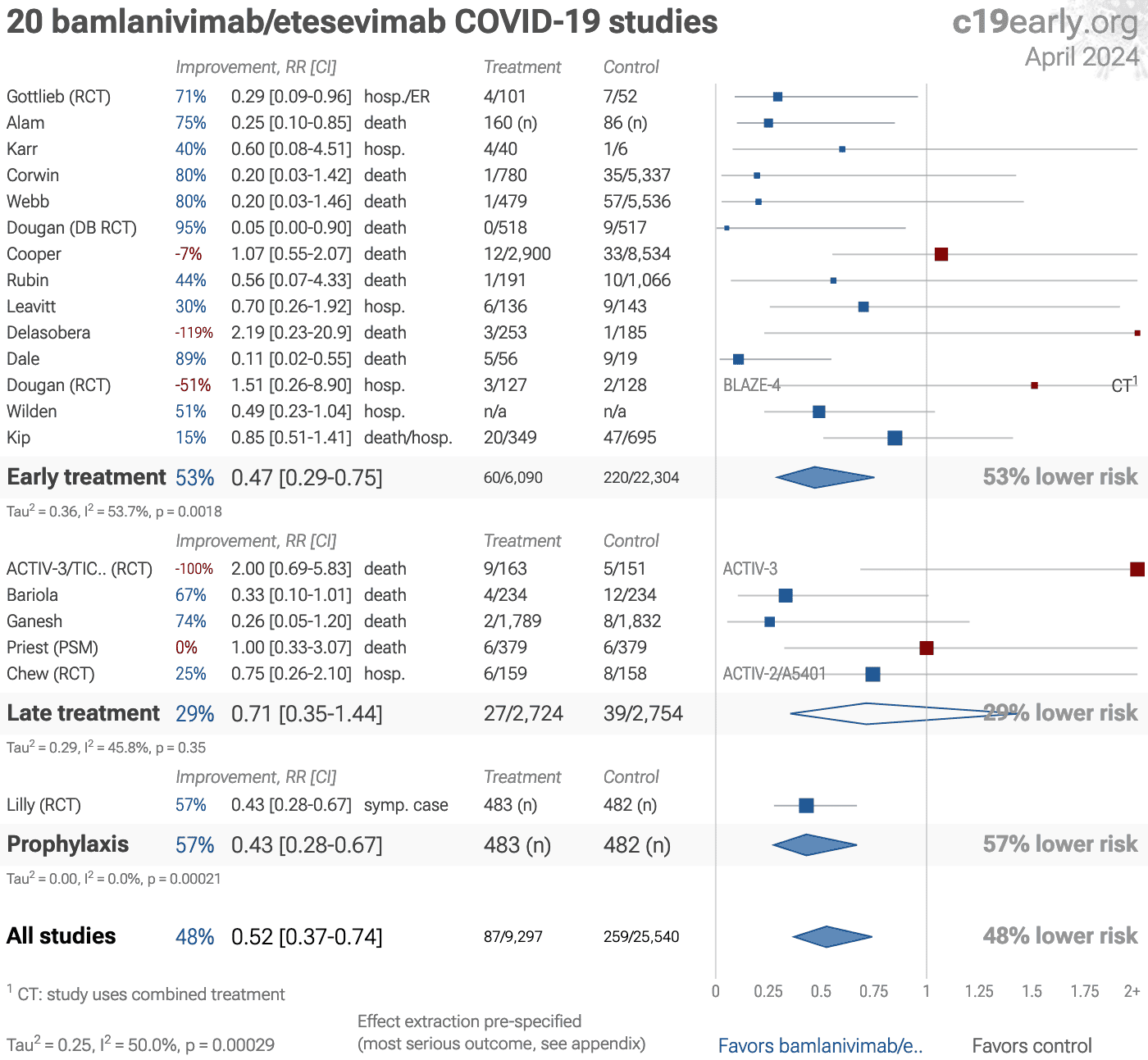
Significantly lower risk is seen for mortality, hospitalization, recovery, cases, and viral clearance. 16 studies from 14 independent teams (all from the same country) show significant benefit.
Meta analysis using the most serious outcome reported shows 46% [24‑61%] lower risk. Results are similar for higher quality and peer-reviewed studies and slightly worse for Randomized Controlled Trials. Results are consistent with early treatment being more effective than late treatment.
Results are robust — in exclusion sensitivity analysis 9 of 22 studies must be excluded to avoid finding statistically significant efficacy in pooled analysis.
Control Bamlanivimab/e..Bamlaniv../e..
Efficacy is highly variant dependent. In Vitro studies suggest a lack of efficacy for omicron1-5. mAb use may create new variants that spread globally6-8, and may be associated with prolonged viral loads, clinical deterioration, and immune escape7,9-12.
Prescription treatments have been preferentially used by patients at lower risk13. Retrospective studies may overestimate efficacy, for example patients with greater knowledge of effective treatments may be more likely to access prescription treatments but result in confounding because they are also more likely to use known beneficial non-prescription treatments.
No treatment is 100% effective. Protocols combine safe and effective options with individual risk/benefit analysis and monitoring. All data and sources to reproduce this analysis are in the appendix.
Amani et al. present another meta analysis for bamlanivimab/etesevimab, showing significant improvements for mortality and hospitalization.
Covid Analysis et al., Dec 2025, preprint, 1 author.