Immunomodulatory effect of bovine lactoferrin during SARS-CoV-2 infection
Andrea Marques Vieira Da Silva, Thiago Lazari Machado, Ryann De Souza Nascimento, Miguel Pires Medeiros Diniz Rodrigues, Felipe Soares Coelho, Luciana Neves Tubarão, Lorenna Carvalho Da Rosa, Camilla Bayma, Vanessa Pimenta Rocha, Ana Beatriz Teixeira Frederico, Jane Silva, Danielle Regina De Almeida De Brito E Cunha, Alessandro Fonseca De Souza, Raphaela Barbosa Gonçalves De Souza, Caroline Augusto Barros, Danielle Da Silva Fiscina, Luiz Claudio Pereira Ribeiro, Carlos Alberto Marques De Carvalho, Bruno Jorge Duque Da Silva, Rodrigo Muller, Tamiris Azamor, Juliana Gil Melgaço, Rafael Braga Gonçalves, Ana Paula Dinis Ano Bom
Frontiers in Immunology, doi:10.3389/fimmu.2024.1456634
Introduction: Lactoferrin (Lf) is an important immunomodulator in infections caused by different agents. During SARS-CoV-2 infection, Lf can hinder or prevent virus access to the intracellular environment. Severe cases of COVID-19 are related to increased production of cytokines, accompanied by a weak type 1 interferon response.
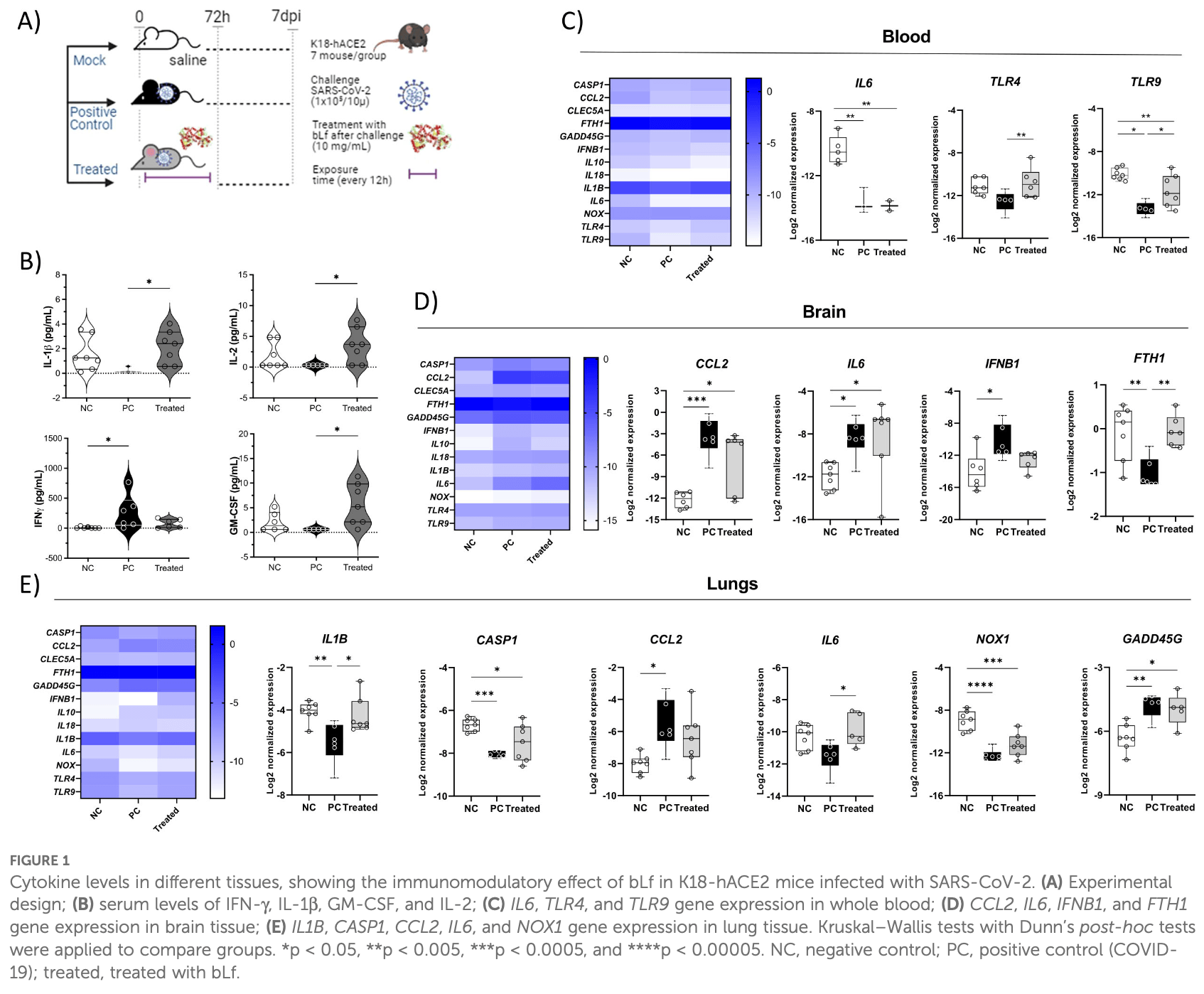
Methods: We investigated the influence of bovine Lf (bLf) in the immune response during SARS-CoV-2 infection in vitro and in vivo assays. Results: Our results show a strong binding between bLf and TLR4/NF-kB in silico, as well as an increase in mRNA expression of these genes in peripheral blood mononuclear cells (PBMCs) treated with bLf. Furthermore, the treatment increased TLR4/TLR9 mRNA expression in infected K18-hACE2 mouse blood, indicating an activation of innate response. Our results show that, when bLf was added, a reduction in the NK cell population was found, presenting a similar effect on PD-1 in TCD4 + and TCD8 + cells. In the culture supernatant of PBMCs from healthy participants, bLf decreased IL-6 levels and increased CCL5 in COVID-19 participants. In addition, K18-hACE2 mice infected and treated with bLf presented an increase of serum pro-inflammatory markers (GM-CSF/IL-1b/ Frontiers in Immunology frontiersin.org 01
Ethics statement The studies involving humans were approved by Institutional Review Board under certificate number 37079320. 4
Conflict of interest The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fimmu.2024.1456634/ full#supplementary-material
References
Alves, Azevedo, Dias, Horbach, Setatino et al., Inhibition of SARS-CoV-2 infection in vero cells by bovine lactoferrin under different iron-saturation states, Pharmaceuticals,
doi:10.3390/ph16101352Ando, Hasegawa, Shindo, Furusawa, Fujino et al., Human lactoferrin activates NF-kB through the Toll-like receptor 4 pathway while it interferes with the lipopolysaccharide-stimulated TLR4 signaling, FEBS J,
doi:10.1111/j.1742-4658.2010.07620.xBerlutti, Pantanella, Natalizi, Frioni, Paesano et al., Antiviral properties of lactoferrin-A natural immunity molecule, Molecules,
doi:10.3390/molecules16086992Bonifacius, Tischer-Zimmermann, Dragon, Gussarow, Vogel et al., COVID-19 immune signatures reveal stable antiviral T cell function despite declining humoral responses, Immunity,
doi:10.1016/j.immuni.2021.01.008Curran, Bertics, Lactoferrin regulates an axis involving CD11b and CD49d integrins and the chemokines MIP-1a and MCP-1 in GM-CSF-treated human primary eosinophils, J Interferon Cytokine Res,
doi:10.1089/jir.2011.0111Fillebeen, Descamps, Dehouck, Fenart, Benaïssa et al., Receptor-mediated transcytosis of lactoferrin through the blood-brain barrier, J Biol Chem,
doi:10.1074/jbc.274.11.7011Fouladseresht, Doroudchi, Rokhtabnak, Abdolrahimzadehfard, Roudgari et al., Predictive monitoring and therapeutic immune biomarkers in the management of clinical complications of COVID-19, Cytokine Growth Factor Rev,
doi:10.1016/j.cytogfr.2020.10.002Guan, Ni, Hu, Liang, Ou et al., Clinical characteristics of coronavirus disease 2019 in China, N Engl J Med,
doi:10.1056/NEJMoa2002032Guerreiro, Robottom-Ferreira, Ribeiro-Alves, Toledo-Pinto, Brito et al., Gene expression profiling specifies chemokine, mitochondrial and lipid metabolism signatures in leprosy, PloS One,
doi:10.1371/journal.pone.0064748Habib, Ibrahim, Zaim, Ibrahim, The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators, Biomed Pharmacother,
doi:10.1016/j.biopha.2021.111228Hadjadj, Yatim, Barnabei, Corneau, Boussier et al., Impaired type I interferon activity and exacerbated inflammatory responses in severe Covid-19 patients, Infect Dis (except HIV/AIDS),
doi:10.1101/2020.04.19.20068015He, Qin, Guan, Liu, Hong et al., Bovine lactoferrin inhibits SARS-CoV-2 and SARS-CoV-1 by targeting the RdRp complex and alleviates viral infection in the hamster model, J Med Virol,
doi:10.1002/jmv.28281Hu, Meng, Zhang, Xiang, Wang, The in vitro antiviral activity of lactoferrin against common human coronaviruses and SARS-CoV-2 is mediated by targeting the heparan sulfate co-receptor, Emerging Microbes Infections,
doi:10.1080/22221751.2021.1888660Hu, Zhang, Cui, Liang, Lu et al., Increasing CCL5/CCR5 on CD4+ T cells in peripheral blood of oral lichen planus, Cytokine,
doi:10.1016/j.cyto.2013.01.020Khan, Khan, Khan, Shal, Rehman et al., Antiinflammatory and anti-rheumatic potential of selective plant compounds by targeting TLR-4/AP-1 signaling: A comprehensive molecular docking and simulation approaches, Molecules,
doi:10.3390/molecules27134319Krämer, Knoll, Bonaguro, Tovinh, Raabe et al., Early IFN-a signatures and persistent dysfunction are distinguishing features of NK cells in severe COVID-19, Immunity,
doi:10.1016/j.immuni.2021.09.002Kuhara, Yamauchi, Tamura, Okamura, Oral administration of lactoferrin increases NK cell activity in mice via increased production of IL-18 and type I IFN in the small intestine, J Interferon Cytokine Res,
doi:10.1089/jir.2006.26.489Lai, Yu, Xian, Ye, Ju et al., Identified human breast milk compositions effectively inhibit SARS-CoV-2 and variants infection and replication, iScience,
doi:10.1016/j.isci.2022.104136Maucourant, Filipovic, Ponzetta, Aleman, Cornillet et al., Natural killer cell immunotypes related to COVID-19 disease severity, Sci Immunol,
doi:10.1126/sciimmunol.abd6832Melgaco, Azamor, Silva, Linhares, Santos et al., Two-step in vitro model to evaluate the cellular immune response to SARS-CoV-2, Cells,
doi:10.3390/cells10092206Melgaco, Brito E Cunha, Azamor, Da Silva, Tubarão et al., Cellular and molecular immunology approaches for the development of immunotherapies against the new coronavirus (SARS-CoV-2): challenges to nearfuture breakthroughs, J Immunol Res,
doi:10.1155/2020/8827670Melgaco, Soriani, Sucupira, Pinheiro, Vieira et al., Changes in cellular proliferation and plasma products are associated with liver failure, World J Hepatol,
doi:10.4254/wjh.v8.i32.1370Montreuil, Tonnelat, Mullet, Preṕaration et proprieteś de la lactosideŕophiline (lactotransferrine) du lait de femme, Biochim Biophys Acta,
doi:10.1016/0006-3002(60)91478-5Mukund, Behera, Alam, Nagaraju, Molecular docking analysis of nuclear factor-kB and genistein interaction in the context of breast cancer, Bioinformation,
doi:10.6026/97320630015011Netea, Rovina, Akinosoglou, Antoniadou, Antonakos, Complex immune dysregulation in COVID-19 patients with severe respiratory failure, Cell Host Microbe,
doi:10.1016/j.chom.2020.04.009Ohradanova-Repic, Skrabana, Gebetsberger, Tajti, Barath et al., Blockade of TMPRSS2-mediated priming of SARS-CoV-2 lactoferricin, Front Immunol,
doi:10.3389/fimmu.2022.958581Ohto, Fukase, Miyake, Shimizu, Structural basis of species-specific endotoxin sensing by innate immune receptor TLR4, Nature,
doi:10.1038/nature11543Okubo, Kamiya, Urano, Nishi, Herter et al., Lactoferrin suppresses neutrophil extracellular traps release in inflammation, EBioMedicine,
doi:10.1016/j.ebiom.2016.07.012Orlov, Wander, Morrell, Mikacenic, Wurfel, A case for targeting th17 cells and IL-17A in SARS-CoV-2 infections, J Immunol,
doi:10.4049/jimmunol.2000554Perdijk, Van Neerven, Van Den Brink, Savelkoul, Brugman, Bovine lactoferrin modulates dendritic cell differentiation and function, Nutrients,
doi:10.3390/nu10070848Peŕez-Garcıá, Martin-Vicente, Rojas-Garcıá, Castilla-Garcıá, Muñoz-Gomez et al., High SARS-CoV-2 viral load and low CCL5 expression levels in the upper respiratory tract are associated with COVID-19 severity, J Infect Dis,
doi:10.1093/infdis/jiab604Prieto-Fernańdez, Egia-Mendikute, Vila-Vecilla, Bosch, Barreira-Manrique et al., Hypoxia reduces cell attachment of SARS-CoV-2 spike protein by modulating the expression of ACE2, neuropilin-1, syndecan-1 and cellular heparan sulfate, Emerging Microbes Infections,
doi:10.1080/22221751.2021.1932607Rascoń-Cruz, Espinoza-Sańchez, Siqueiros-Cendoń, Nakamura-Bencomo, Arevalo-Gallegos et al., Lactoferrin: A glycoprotein involved in immunomodulation, anticancer, and antimicrobial processes, Molecules,
doi:10.3390/molecules26010205Redwan, Uversky, El-Fakharany, Al-Mehdar, Potential lactoferrin activity against pathogenic viruses, Comptes Rendus Biologies,
doi:10.1016/j.crvi.2014.08.003Rosa, Cutone, Lepanto, Paesano, Valenti, Lactoferrin: A natural glycoprotein involved in iron and inflammatory homeostasis, IJMS,
doi:10.3390/ijms18091985Tang, Li, Wang, Sun, Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia, J Thromb Haemost,
doi:10.1111/jth.14768Valenti, Antonini, Lactoferrin: Lactoferrin: an important host defence against microbial and viral attack, Cell Mol Life Sci,
doi:10.1007/s00018-005-5372-0Vasireddy, Vanaparthy, Mohan, Malayala, Atluri, Review of COVID-19 variants and COVID-19 vaccine efficacy: what the clinician should know?, J Clin Med Res,
doi:10.14740/jocmr4518Wang, Wang, Wang, Luo, Wan et al., Lactoferrin for the treatment of COVID-19 (Review), Exp Ther Med,
doi:10.3892/etm.2020.9402Who, Coronavirus (COVID-19) dashboard
Wotring, Fursmidt, Ward, Sexton, Evaluating the in vitro efficacy of bovine lactoferrin products against SARS-CoV-2 variants of concern, J Dairy Sci,
doi:10.3168/jds.2021-21247Xavier, Silva, Almeida, Conceicão, Lacerda et al., COVID-19: clinical and laboratory manifestations in novel coronavirus infection, Jornal Brasileiro Patologia e Medicina Laboratorial,
doi:10.5935/1676-2444.20200049Zemankova, Chlebova, Matiasovic, Prodelalova, Gebauer et al., Bovine lactoferrin free of lipopolysaccharide can induce a proinflammatory response of macrophages, BMC Vet Res,
doi:10.1186/s12917-016-0878-2Zeng, Xu, Xie, Yan, Xie et al., Pulmonary pathology of early phase COVID-19 pneumonia in a patient with a benign lung lesion, Histopathology,
doi:10.1111/his.14138Zhao, Li, Yu, Wu, Ding et al., Identification of lactoferrin-derived peptides as potential inhibitors against the main protease of SARS-CoV-2, Lebensm Wiss Technol,
doi:10.1016/j.lwt.2021.112684Zhao, Yuan, Wang, Liu, Liao et al., Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019, Clin Infect Dis,
doi:10.1093/cid/ciaa344{ 'indexed': { 'date-parts': [[2024, 10, 18]],
'date-time': '2024-10-18T04:12:53Z',
'timestamp': 1729224773032,
'version': '3.27.0'},
'reference-count': 51,
'publisher': 'Frontiers Media SA',
'license': [ { 'start': { 'date-parts': [[2024, 10, 17]],
'date-time': '2024-10-17T00:00:00Z',
'timestamp': 1729123200000},
'content-version': 'vor',
'delay-in-days': 0,
'URL': 'https://creativecommons.org/licenses/by/4.0/'}],
'content-domain': {'domain': ['frontiersin.org'], 'crossmark-restriction': True},
'abstract': '<jats:sec><jats:title>Introduction</jats:title><jats:p>Lactoferrin (Lf) is an important '
'immunomodulator in infections caused by different agents. During SARS-CoV-2 infection, Lf can '
'hinder or prevent virus access to the intracellular environment. Severe cases of COVID-19 are '
'related to increased production of cytokines, accompanied by a weak type 1 interferon '
'response.</jats:p></jats:sec><jats:sec><jats:title>Methods</jats:title><jats:p>We '
'investigated the influence of bovine Lf (bLf) in the immune response during SARS-CoV-2 '
'infection <jats:italic>in vitro</jats:italic> and <jats:italic>in vivo</jats:italic> '
'assays.</jats:p></jats:sec><jats:sec><jats:title>Results</jats:title><jats:p>Our results show '
'a strong binding between bLf and TLR4/NF-κB <jats:italic>in silico</jats:italic>, as well as '
'an increase in mRNA expression of these genes in peripheral blood mononuclear cells (PBMCs) '
'treated with bLf. Furthermore, the treatment increased <jats:italic>TLR4/TLR9</jats:italic> '
'mRNA expression in infected K18-hACE2 mouse blood, indicating an activation of innate '
'response. Our results show that, when bLf was added, a reduction in the NK cell population '
'was found, presenting a similar effect on PD-1 in TCD4<jats:sup>+</jats:sup> and '
'TCD8<jats:sup>+</jats:sup> cells. In the culture supernatant of PBMCs from healthy '
'participants, bLf decreased IL-6 levels and increased CCL5 in COVID-19 participants. In '
'addition, K18-hACE2 mice infected and treated with bLf presented an increase of serum '
'pro-inflammatory markers (GM-CSF/IL-1β/IL-2) and upregulated mRNA expression of '
'<jats:italic>IL1B</jats:italic> and <jats:italic>IL6</jats:italic> in the lung tissue. '
'Furthermore, bLf treatment was able to restore <jats:italic>FTH1</jats:italic> levels in '
'brain tissue.</jats:p></jats:sec><jats:sec><jats:title>Discussion</jats:title><jats:p>The '
'data indicate that bLf can be part of a therapeutic strategy to promote the immunomodulation '
'effect, leading to homeostasis during COVID-19.</jats:p></jats:sec>',
'DOI': '10.3389/fimmu.2024.1456634',
'type': 'journal-article',
'created': { 'date-parts': [[2024, 10, 17]],
'date-time': '2024-10-17T04:45:35Z',
'timestamp': 1729140335000},
'update-policy': 'http://dx.doi.org/10.3389/crossmark-policy',
'source': 'Crossref',
'is-referenced-by-count': 0,
'title': 'Immunomodulatory effect of bovine lactoferrin during SARS-CoV-2 infection',
'prefix': '10.3389',
'volume': '15',
'author': [ { 'given': 'Andrea Marques Vieira da',
'family': 'Silva',
'sequence': 'first',
'affiliation': []},
{'given': 'Thiago Lazari', 'family': 'Machado', 'sequence': 'additional', 'affiliation': []},
{ 'given': 'Ryann de Souza',
'family': 'Nascimento',
'sequence': 'additional',
'affiliation': []},
{ 'given': 'Miguel Pires Medeiros Diniz',
'family': 'Rodrigues',
'sequence': 'additional',
'affiliation': []},
{'given': 'Felipe Soares', 'family': 'Coelho', 'sequence': 'additional', 'affiliation': []},
{'given': 'Luciana Neves', 'family': 'Tubarão', 'sequence': 'additional', 'affiliation': []},
{'given': 'Lorenna Carvalho', 'family': 'da Rosa', 'sequence': 'additional', 'affiliation': []},
{'given': 'Camilla', 'family': 'Bayma', 'sequence': 'additional', 'affiliation': []},
{'given': 'Vanessa Pimenta', 'family': 'Rocha', 'sequence': 'additional', 'affiliation': []},
{ 'given': 'Ana Beatriz Teixeira',
'family': 'Frederico',
'sequence': 'additional',
'affiliation': []},
{'given': 'Jane', 'family': 'Silva', 'sequence': 'additional', 'affiliation': []},
{ 'given': 'Danielle Regina de Almeida de Brito e',
'family': 'Cunha',
'sequence': 'additional',
'affiliation': []},
{ 'given': 'Alessandro Fonseca',
'family': 'de Souza',
'sequence': 'additional',
'affiliation': []},
{ 'given': 'Raphaela Barbosa Gonçalves de',
'family': 'Souza',
'sequence': 'additional',
'affiliation': []},
{'given': 'Caroline Augusto', 'family': 'Barros', 'sequence': 'additional', 'affiliation': []},
{ 'given': 'Danielle da Silva',
'family': 'Fiscina',
'sequence': 'additional',
'affiliation': []},
{ 'given': 'Luiz Claudio Pereira',
'family': 'Ribeiro',
'sequence': 'additional',
'affiliation': []},
{ 'given': 'Carlos Alberto Marques',
'family': 'de Carvalho',
'sequence': 'additional',
'affiliation': []},
{ 'given': 'Bruno Jorge Duque',
'family': 'da Silva',
'sequence': 'additional',
'affiliation': []},
{'given': 'Rodrigo', 'family': 'Muller', 'sequence': 'additional', 'affiliation': []},
{'given': 'Tamiris', 'family': 'Azamor', 'sequence': 'additional', 'affiliation': []},
{'given': 'Juliana Gil', 'family': 'Melgaço', 'sequence': 'additional', 'affiliation': []},
{'given': 'Rafael Braga', 'family': 'Gonçalves', 'sequence': 'additional', 'affiliation': []},
{'given': 'Ana Paula Dinis', 'family': 'Ano Bom', 'sequence': 'additional', 'affiliation': []}],
'member': '1965',
'published-online': {'date-parts': [[2024, 10, 17]]},
'reference': [ {'key': 'B1', 'unstructured': 'Coronavirus (COVID-19) dashboard'},
{ 'key': 'B2',
'doi-asserted-by': 'publisher',
'first-page': 'e3232020',
'DOI': '10.5935/1676-2444.20200049',
'article-title': 'COVID-19: clinical and laboratory manifestations in novel coronavirus '
'infection',
'volume': '56',
'author': 'Xavier',
'year': '2020',
'journal-title': 'Jornal Brasileiro Patologia e Medicina Laboratorial'},
{ 'key': 'B3',
'doi-asserted-by': 'publisher',
'DOI': '10.1111/jth.14768',
'article-title': 'Abnormal coagulation parameters are associated with poor prognosis in '
'patients with novel coronavirus pneumonia',
'volume': '18',
'author': 'Tang',
'year': '2020',
'journal-title': 'J Thromb Haemost'},
{ 'key': 'B4',
'doi-asserted-by': 'publisher',
'DOI': '10.1155/2020/8827670',
'article-title': 'Cellular and molecular immunology approaches for the development of '
'immunotherapies against the new coronavirus (SARS-CoV-2): challenges to '
'near-future breakthroughs',
'volume': '2020',
'author': 'Melgaço',
'year': '2020',
'journal-title': 'J Immunol Res'},
{ 'key': 'B5',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.ebiom.2016.07.012',
'article-title': 'Lactoferrin suppresses neutrophil extracellular traps release in '
'inflammation',
'volume': '10',
'author': 'Okubo',
'year': '2016',
'journal-title': 'EBioMedicine'},
{ 'key': 'B6',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/0006-3002(60)91478-5',
'article-title': 'Préparation et propriétés de la lactosidérophiline (lactotransferrine) '
'du lait de femme',
'volume': '45',
'author': 'Montreuil',
'year': '1960',
'journal-title': 'Biochim Biophys Acta'},
{ 'key': 'B7',
'doi-asserted-by': 'publisher',
'DOI': '10.1139/o2012-016',
'article-title': 'Lactoferrin, a bird’s eye view',
'volume': '90',
'author': 'Vogel',
'year': '2012',
'journal-title': 'Biochem Cell Biol'},
{ 'key': 'B8',
'doi-asserted-by': 'publisher',
'DOI': '10.1007/s00018-005-5372-0',
'article-title': 'Lactoferrin: Lactoferrin: an important host defence against microbial '
'and viral attack',
'volume': '62',
'author': 'Valenti',
'year': '2005',
'journal-title': 'Cell Mol Life Sci'},
{ 'key': 'B9',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.biochi.2008.05.005',
'article-title': 'Immunomodulatory effects of lactoferrin on antigen presenting cells',
'volume': '91',
'author': 'Puddu',
'year': '2009',
'journal-title': 'Biochimie'},
{ 'key': 'B10',
'doi-asserted-by': 'publisher',
'DOI': '10.3390/ijms18091985',
'article-title': 'Lactoferrin: A natural glycoprotein involved in iron and inflammatory '
'homeostasis',
'volume': '18',
'author': 'Rosa',
'year': '2017',
'journal-title': 'IJMS'},
{ 'key': 'B11',
'doi-asserted-by': 'publisher',
'first-page': '6992',
'DOI': '10.3390/molecules16086992',
'article-title': 'Antiviral properties of lactoferrin—A natural immunity molecule',
'volume': '16',
'author': 'Berlutti',
'year': '2011',
'journal-title': 'Molecules'},
{ 'key': 'B12',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.crvi.2014.08.003',
'article-title': 'Potential lactoferrin activity against pathogenic viruses',
'volume': '337',
'author': 'Redwan',
'year': '2014',
'journal-title': 'Comptes Rendus Biologies'},
{ 'key': 'B13',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.ijantimicag.2020.106118',
'article-title': 'Lactoferrin as potential preventative and adjunct treatment for '
'COVID-19',
'volume': '56',
'author': 'Chang',
'year': '2020',
'journal-title': 'Int J Antimicrobial Agents'},
{ 'key': 'B14',
'doi-asserted-by': 'publisher',
'DOI': '10.3168/jds.2021-21247',
'article-title': 'Evaluating the in vitro efficacy of bovine lactoferrin products against '
'SARS-CoV-2 variants of concern',
'volume': '105',
'author': 'Wotring',
'year': '2022',
'journal-title': 'J Dairy Sci'},
{ 'key': 'B15',
'doi-asserted-by': 'publisher',
'DOI': '10.1089/jir.2006.26.489',
'article-title': 'Oral administration of lactoferrin increases NK cell activity in mice '
'via increased production of IL-18 and type I IFN in the small intestine',
'volume': '26',
'author': 'Kuhara',
'year': '2006',
'journal-title': 'J Interferon Cytokine Res'},
{ 'key': 'B16',
'doi-asserted-by': 'publisher',
'DOI': '10.3390/molecules26010205',
'article-title': 'Lactoferrin: A glycoprotein involved in immunomodulation, anticancer, '
'and antimicrobial processes',
'volume': '26',
'author': 'Rascón-Cruz',
'year': '2021',
'journal-title': 'Molecules'},
{ 'key': 'B17',
'doi-asserted-by': 'publisher',
'DOI': '10.1089/jir.2011.0111',
'article-title': 'Lactoferrin regulates an axis involving CD11b and CD49d integrins and '
'the chemokines MIP-1α and MCP-1 in GM-CSF-treated human primary '
'eosinophils',
'volume': '32',
'author': 'Curran',
'year': '2012',
'journal-title': 'J Interferon Cytokine Res'},
{ 'key': 'B18',
'doi-asserted-by': 'publisher',
'first-page': '251',
'DOI': '10.1186/s12917-016-0878-2',
'article-title': 'Bovine lactoferrin free of lipopolysaccharide can induce a '
'proinflammatory response of macrophages',
'volume': '12',
'author': 'Zemankova',
'year': '2016',
'journal-title': 'BMC Vet Res'},
{ 'key': 'B19',
'doi-asserted-by': 'publisher',
'DOI': '10.3390/molecules27134319',
'article-title': 'Anti-inflammatory and anti-rheumatic potential of selective plant '
'compounds by targeting TLR-4/AP-1 signaling: A comprehensive molecular '
'docking and simulation approaches',
'volume': '27',
'author': 'Khan',
'year': '2022',
'journal-title': 'Molecules'},
{ 'key': 'B20',
'doi-asserted-by': 'publisher',
'DOI': '10.1056/NEJMoa2002032',
'article-title': 'Clinical characteristics of coronavirus disease 2019 in China',
'volume': '382',
'author': 'Guan',
'year': '2020',
'journal-title': 'N Engl J Med'},
{ 'key': 'B21',
'doi-asserted-by': 'publisher',
'DOI': '10.1126/sciimmunol.abd6832',
'article-title': 'Natural killer cell immunotypes related to COVID-19 disease severity',
'volume': '5',
'author': 'Maucourant',
'year': '2020',
'journal-title': 'Sci Immunol'},
{ 'key': 'B22',
'doi-asserted-by': 'publisher',
'first-page': '823-31',
'DOI': '10.1111/his.14138',
'article-title': 'Pulmonary pathology of early phase COVID-19 pneumonia in a patient with '
'a benign lung lesion',
'volume': '5',
'author': 'Zeng',
'year': '2020',
'journal-title': 'Histopathology'},
{ 'key': 'B23',
'doi-asserted-by': 'publisher',
'first-page': 'ciaa344',
'DOI': '10.1093/cid/ciaa344',
'article-title': 'Antibody responses to SARS-CoV-2 in patients of novel coronavirus '
'disease 2019',
'author': 'Zhao',
'year': '2020',
'journal-title': 'Clin Infect Dis'},
{ 'key': 'B24',
'doi-asserted-by': 'publisher',
'first-page': '340',
'DOI': '10.1016/j.immuni.2021.01.008',
'article-title': 'COVID-19 immune signatures reveal stable antiviral T cell function '
'despite declining humoral responses',
'volume': '54',
'author': 'Bonifacius',
'year': '2021',
'journal-title': 'Immunity'},
{ 'key': 'B25',
'doi-asserted-by': 'publisher',
'DOI': '10.4254/wjh.v8.i32.1370',
'article-title': 'Changes in cellular proliferation and plasma products are associated '
'with liver failure',
'volume': '8',
'author': 'Melgaço',
'year': '2016',
'journal-title': 'World J Hepatol'},
{ 'key': 'B26',
'doi-asserted-by': 'publisher',
'DOI': '10.1371/journal.pone.0064748',
'article-title': 'Gene expression profiling specifies chemokine, mitochondrial and lipid '
'metabolism signatures in leprosy',
'volume': '8',
'author': 'Guerreiro',
'year': '2013',
'journal-title': 'PloS One'},
{ 'key': 'B27',
'doi-asserted-by': 'publisher',
'DOI': '10.14740/jocmr4518',
'article-title': 'Review of COVID-19 variants and COVID-19 vaccine efficacy: what the '
'clinician should know',
'volume': '13',
'author': 'Vasireddy',
'year': '2021',
'journal-title': 'J Clin Med Res'},
{ 'key': 'B28',
'doi-asserted-by': 'publisher',
'DOI': '10.1002/rmv.2313',
'article-title': 'Covid-19 vaccines and variants of concern: A review',
'volume': '32',
'author': 'Hadj Hassine',
'year': '2022',
'journal-title': 'Rev Med Virol'},
{ 'key': 'B29',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.biopha.2021.111228',
'article-title': 'The role of iron in the pathogenesis of COVID-19 and possible treatment '
'with lactoferrin and other iron chelators',
'volume': '136',
'author': 'Habib',
'year': '2021',
'journal-title': 'Biomed Pharmacother'},
{ 'key': 'B30',
'doi-asserted-by': 'publisher',
'first-page': '1',
'DOI': '10.3892/etm.2020.9402',
'article-title': 'Lactoferrin for the treatment of COVID−19 (Review)',
'volume': '20',
'author': 'Wang',
'year': '2020',
'journal-title': 'Exp Ther Med'},
{ 'key': 'B31',
'doi-asserted-by': 'publisher',
'first-page': '32',
'DOI': '10.1016/j.cytogfr.2020.10.002',
'article-title': 'Predictive monitoring and therapeutic immune biomarkers in the '
'management of clinical complications of COVID-19',
'volume': '58',
'author': 'Fouladseresht',
'year': '2021',
'journal-title': 'Cytokine Growth Factor Rev'},
{ 'key': 'B32',
'doi-asserted-by': 'publisher',
'DOI': '10.3390/nu10070848',
'article-title': 'Bovine lactoferrin modulates dendritic cell differentiation and '
'function',
'volume': '10',
'author': 'Perdijk',
'year': '2018',
'journal-title': 'Nutrients'},
{ 'key': 'B33',
'doi-asserted-by': 'publisher',
'DOI': '10.1038/nature11543',
'article-title': 'Structural basis of species-specific endotoxin sensing by innate immune '
'receptor TLR4',
'volume': '490',
'author': 'Ohto',
'year': '2012',
'journal-title': 'Nature'},
{ 'key': 'B34',
'doi-asserted-by': 'publisher',
'DOI': '10.6026/97320630015011',
'article-title': 'Molecular docking analysis of nuclear factor-κB and genistein '
'interaction in the context of breast cancer',
'volume': '15',
'author': 'Mukund',
'year': '2019',
'journal-title': 'Bioinformation'},
{ 'key': 'B35',
'doi-asserted-by': 'publisher',
'first-page': '718-24',
'DOI': '10.1101/2020.04.19.20068015',
'article-title': 'Impaired type I interferon activity and exacerbated inflammatory '
'responses in severe Covid-19 patients',
'volume': '369',
'author': 'Hadjadj',
'year': '2020',
'journal-title': 'Infect Dis (except HIV/AIDS)'},
{ 'key': 'B36',
'doi-asserted-by': 'publisher',
'DOI': '10.1111/j.1742-4658.2010.07620.x',
'article-title': 'Human lactoferrin activates NF-κB through the Toll-like receptor 4 '
'pathway while it interferes with the lipopolysaccharide-stimulated TLR4 '
'signaling',
'volume': '277',
'author': 'Ando',
'year': '2010',
'journal-title': 'FEBS J'},
{ 'key': 'B37',
'doi-asserted-by': 'publisher',
'DOI': '10.3390/cells10092206',
'article-title': 'Two-step in vitro model to evaluate the cellular immune response to '
'SARS-CoV-2',
'volume': '10',
'author': 'Melgaço',
'year': '2021',
'journal-title': 'Cells'},
{ 'key': 'B38',
'doi-asserted-by': 'publisher',
'DOI': '10.4049/jimmunol.2000554',
'article-title': 'A case for targeting th17 cells and IL-17A in SARS-CoV-2 infections',
'volume': '205',
'author': 'Orlov',
'year': '2020',
'journal-title': 'J Immunol'},
{ 'key': 'B39',
'doi-asserted-by': 'publisher',
'DOI': '10.3390/cells10061550',
'article-title': 'The role of th17 response in COVID-19',
'volume': '10',
'author': 'Martonik',
'year': '2021',
'journal-title': 'Cells'},
{ 'key': 'B40',
'doi-asserted-by': 'publisher',
'first-page': '992',
'DOI': '10.1016/j.chom.2020.04.009',
'article-title': 'Complex immune dysregulation in COVID-19 patients with severe '
'respiratory failure',
'volume': '27',
'author': 'Giamarellos-Bourboulis',
'year': '2020',
'journal-title': 'Cell Host Microbe'},
{ 'key': 'B41',
'doi-asserted-by': 'publisher',
'first-page': '2650',
'DOI': '10.1016/j.immuni.2021.09.002',
'article-title': 'Early IFN-α signatures and persistent dysfunction are distinguishing '
'features of NK cells in severe COVID-19',
'volume': '54',
'author': 'Krämer',
'year': '2021',
'journal-title': 'Immunity'},
{ 'key': 'B42',
'doi-asserted-by': 'publisher',
'DOI': '10.1093/infdis/jiab604',
'article-title': 'High SARS-CoV-2 viral load and low CCL5 expression levels in the upper '
'respiratory tract are associated with COVID-19 severity',
'volume': '225',
'author': 'Pérez-García',
'year': '2022',
'journal-title': 'J Infect Dis'},
{ 'key': 'B43',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.cyto.2013.01.020',
'article-title': 'Increasing CCL5/CCR5 on CD4+ T cells in peripheral blood of oral lichen '
'planus',
'volume': '62',
'author': 'Hu',
'year': '2013',
'journal-title': 'Cytokine'},
{ 'key': 'B44',
'doi-asserted-by': 'publisher',
'DOI': '10.1074/jbc.274.11.7011',
'article-title': 'Receptor-mediated transcytosis of lactoferrin through the blood-brain '
'barrier',
'volume': '274',
'author': 'Fillebeen',
'year': '1999',
'journal-title': 'J Biol Chem'},
{ 'key': 'B45',
'doi-asserted-by': 'publisher',
'DOI': '10.1080/22221751.2021.1888660',
'article-title': 'The in vitro antiviral activity of lactoferrin against common human '
'coronaviruses and SARS-CoV-2 is mediated by targeting the heparan '
'sulfate co-receptor',
'volume': '10',
'author': 'Hu',
'year': '2021',
'journal-title': 'Emerging Microbes Infections'},
{ 'key': 'B46',
'doi-asserted-by': 'publisher',
'DOI': '10.1080/22221751.2021.1932607',
'article-title': 'Hypoxia reduces cell attachment of SARS-CoV-2 spike protein by '
'modulating the expression of ACE2, neuropilin-1, syndecan-1 and '
'cellular heparan sulfate',
'volume': '10',
'author': 'Prieto-Fernández',
'year': '2021',
'journal-title': 'Emerging Microbes Infections'},
{ 'key': 'B47',
'doi-asserted-by': 'publisher',
'DOI': '10.3389/fimmu.2022.958581',
'article-title': 'Blockade of TMPRSS2-mediated priming of SARS-CoV-2 by lactoferricin',
'volume': '13',
'author': 'Ohradanova-Repic',
'year': '2022',
'journal-title': 'Front Immunol'},
{ 'key': 'B48',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.isci.2022.104136',
'article-title': 'Identified human breast milk compositions effectively inhibit '
'SARS-CoV-2 and variants infection and replication',
'volume': '25',
'author': 'Lai',
'year': '2022',
'journal-title': 'iScience'},
{ 'key': 'B49',
'doi-asserted-by': 'publisher',
'DOI': '10.1002/jmv.28281',
'article-title': 'Bovine lactoferrin inhibits SARS-CoV-2 and SARS-CoV-1 by targeting the '
'RdRp complex and alleviates viral infection in the hamster model',
'volume': '95',
'author': 'He',
'year': '2023',
'journal-title': 'J Med Virol'},
{ 'key': 'B50',
'doi-asserted-by': 'publisher',
'DOI': '10.1016/j.lwt.2021.112684',
'article-title': 'Identification of lactoferrin-derived peptides as potential inhibitors '
'against the main protease of SARS-CoV-2',
'volume': '154',
'author': 'Zhao',
'year': '2022',
'journal-title': 'Lebensm Wiss Technol'},
{ 'key': 'B51',
'doi-asserted-by': 'publisher',
'DOI': '10.3390/ph16101352',
'article-title': 'Inhibition of SARS-CoV-2 infection in vero cells by bovine lactoferrin '
'under different iron-saturation states',
'volume': '16',
'author': 'Alves',
'year': '2023',
'journal-title': 'Pharmaceuticals'}],
'container-title': 'Frontiers in Immunology',
'original-title': [],
'link': [ { 'URL': 'https://www.frontiersin.org/articles/10.3389/fimmu.2024.1456634/full',
'content-type': 'unspecified',
'content-version': 'vor',
'intended-application': 'similarity-checking'}],
'deposited': { 'date-parts': [[2024, 10, 17]],
'date-time': '2024-10-17T04:45:39Z',
'timestamp': 1729140339000},
'score': 1,
'resource': {'primary': {'URL': 'https://www.frontiersin.org/articles/10.3389/fimmu.2024.1456634/full'}},
'subtitle': [],
'short-title': [],
'issued': {'date-parts': [[2024, 10, 17]]},
'references-count': 51,
'alternative-id': ['10.3389/fimmu.2024.1456634'],
'URL': 'http://dx.doi.org/10.3389/fimmu.2024.1456634',
'relation': {},
'ISSN': ['1664-3224'],
'subject': [],
'container-title-short': 'Front. Immunol.',
'published': {'date-parts': [[2024, 10, 17]]}}